Self-care has emerged as a critical component in modern healthcare, playing a vital role in preventing, managing, and rehabilitating a wide spectrum of health conditions, including the growing global burden of chronic non-communicable diseases. Recognizing the significance of individual self-care capabilities, numerous tools have been developed to measure these capacities in adults across various health statuses, from healthy individuals to those managing chronic conditions. However, the landscape of Self Care Assessment Tools is diverse, and a comprehensive overview of non-disease-specific tools has been lacking. This article addresses this gap by providing an in-depth analysis of the existing non-mono-disease specific self care assessment tools available for adults, aiming to offer a clearer understanding of their characteristics, content, and potential applications.
Background: The Rising Need for Self Care Assessment
The increasing prevalence of chronic diseases, often linked to lifestyle factors, underscores the importance of effective self-care practices. Conditions such as type 2 diabetes, cardiovascular disease, and certain cancers are significantly influenced by an individual’s ability to engage in self-care. The World Health Organization (WHO) has emphasized self-care’s importance through guidelines in 2019 and 2021, defining it as “the ability of individuals, families and communities to promote health, prevent diseases, maintain health, and to cope with illness and disability with or without the support of a healthcare provider.” This broad definition encompasses a wide array of behaviors and decisions related to lifestyle, hygiene, environment, and socioeconomic factors, all impacting physical and mental well-being.
To provide a structured approach to understanding self-care, the ‘Seven Pillars of Self-Care’ (7PSC) framework was developed. This framework highlights seven essential domains: (i) knowledge and health literacy, (ii) mental wellbeing, self-awareness and agency, (iii) physical activity, (iv) healthy eating, (v) risk avoidance and mitigation, (vi) good hygiene, and (vii) the rational use of products and services. The 7PSC framework serves as a valuable benchmark for evaluating self-care practices and initiatives, offering a comprehensive perspective beyond disease-specific self-management.
Measuring an individual’s capacity for self-care is becoming increasingly crucial as healthcare systems globally recognize self-care as a cornerstone of achieving “health for all.” Policymakers are actively investing in public health programs aimed at promoting self-care and self-management. To effectively assess the impact of these interventions, reliable and valid self care assessment tools are necessary. However, the field is characterized by a multitude of tools, varying definitions of “self-care,” and a lack of clarity regarding the specific aspects of self-care each tool measures. Many existing tools focus on specific conditions or populations, leaving a gap in comprehensive, non-disease-specific assessments.
While some tools explicitly use the term “self-care,” others, like the Patient Activation Measure, act as proxy-measures, assessing related concepts such as “patient activation” or “self-management.” Previous reviews have examined self-care measurement tools, but often with a focus on condition-specific instruments or excluding assessments by healthcare professionals. This review aims to bridge this knowledge gap by systematically identifying and characterizing various self care assessment tools for adults that are not specific to a single disease. The secondary objectives include analyzing these tools’ content, structure, psychometric properties, and alignment with the 7PSC framework, providing a comprehensive evaluation of the current landscape of self care assessment tools.
Methods: A Scoping Review Approach to Identifying Self Care Assessment Tools
This review adopted a scoping review methodology, guided by the PRISMA extension for scoping reviews, to systematically identify, evaluate, and map the landscape of self care assessment tools designed for adults. The focus was on tools assessing health literacy, capability, and/or performance related to general health self-care practices. Both self-reported and observer-based data collection methods were considered for inclusion. The review targeted tools applicable to adults, measuring self-care either as the primary focus or as a significant component. Tools focusing on “self-management” were also included to capture a broader spectrum of relevant assessments. To ensure relevance and rigor, only peer-reviewed articles published in English between January 1, 1950, and November 30, 2022, were considered.
Specific exclusion criteria were applied to refine the scope. Tools designed solely for disease-specific self-care management or for specific medical settings or themes (e.g., blood pressure monitoring alone) were excluded to maintain the focus on non-disease-specific self care assessment tools. Tools presented only in abstracts or conference proceedings were also excluded to ensure access to full methodological details.
The search strategy was meticulously developed in consultation with a research librarian to ensure comprehensive coverage. Initial searches in MEDLINE and Embase helped refine search terms and confirm result relevance. Manual searching of reference lists from relevant studies and similar reviews further expanded the search. Subject headings were adapted for each database to maximize retrieval.
Database searches were conducted on December 1, 2022, covering the period from January 1, 1950, to November 30, 2022. Four key databases were searched: Embase, PubMed, PsycINFO, and CINAHL. Search terms included a combination of MeSH terms and keywords such as (“self-care” OR “self-management” OR “self-monitoring” OR “self-assessment”) AND (adult*) AND (“instrument*” OR “questionnaire*” OR “scale*” OR “assessment’’). Detailed search strategies for each database are available in supplementary materials. While no manual searching was performed beyond reference screening, the references of all included studies were thoroughly reviewed to identify additional relevant tools. Throughout this review, the term “tool” is used as an umbrella term encompassing instruments, scales, questionnaires, and assessments.
Study selection involved a rigorous multi-stage process. Retrieved studies were initially imported into Endnote X7 to remove duplicates. Covidence software was then used for further duplicate removal and screening. Titles and abstracts were screened by two researchers independently. Full texts of potentially eligible studies were then assessed independently by two researchers. Disagreements between primary reviewers were resolved by a third researcher, and any remaining discrepancies were addressed through team discussions.
The primary aim was to identify tools, not just studies. Therefore, the screening process focused on articles describing or using self care assessment tools. Once eligible tools were identified, “primary reference” studies, which were the initial publications describing the tool’s development, testing, and intended use, were sought. In cases of tool revisions, publications detailing these revisions were also included to ensure the most up-to-date information was captured.
Data extraction, following full-text screening, was conducted by a single researcher for each tool using a standardized extraction form based on the identified “primary reference.” Extracted data included a brief tool description, reference study authors, year of publication, country of origin, tool aims (prevention, rehabilitation, management), validity and reliability testing, number of items, scoring system, scale type, administration method (self-reported and/or observer-reported), and score interpretation. The time required to complete each self care assessment tool was also recorded, or estimated based on item count, assuming 6 seconds per item for self-completion and 10 seconds for completion by a healthcare professional.
A qualitative content assessment was performed for each identified self care assessment tool using the 7PSC framework. This framework guided the analysis by evaluating the extent to which each tool captured information relevant to each of the seven pillars. A Black, Red, Amber, and Green (BRAG) traffic light system was used to score each tool’s coverage of each pillar. Black indicated the tool was unavailable for review (score = 0), Red indicated the pillar was not addressed (score = 0), Amber indicated partial coverage of the pillar (at least one relevant item), and Green indicated explicit and comprehensive coverage of the pillar (score = 1). This analysis resulted in a configuration matrix characterizing the various self care assessment tools used for adults in non-mono-disease-specific or non-medicalized settings.
Results: Overview of Identified Self Care Assessment Tools
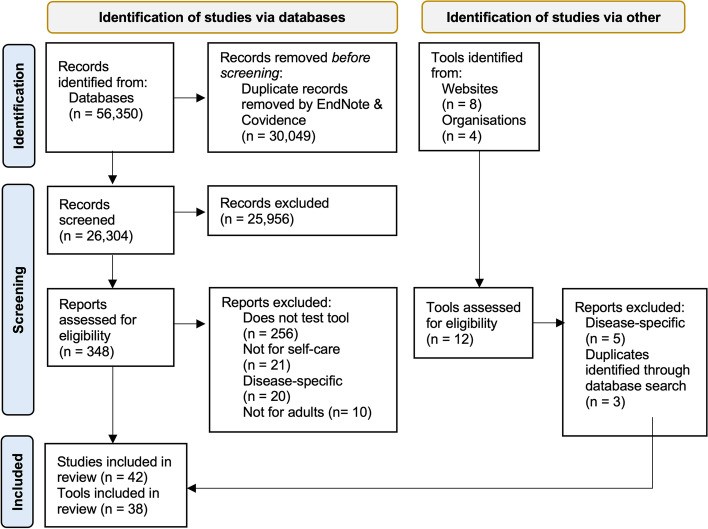
The systematic search and screening process identified 38 distinct self care assessment tools, described across 42 primary reference studies, that met the inclusion criteria (Fig. 1).
Figure 1: PRISMA Flowchart
A significant majority of these tools (n = 26; 68.4%) originated from North America, with 24 from the USA and two from Canada. The remaining tools were developed in the UK, Norway, Spain, Finland, the Netherlands, and Italy, highlighting a global interest in self care assessment. Notably, four tools (EQ-5D, SASS-14, SSCII, and SASE) were the result of international collaborations, indicating a growing trend towards cross-cultural and internationally applicable self care assessment tools.
Table 1 provides a detailed overview of the key characteristics of these 38 self care assessment tools, including their year of publication, origin, brief description, intended stage of application (prevention, rehabilitation, or management), target population, number of items, estimated completion time, completion method, and scoring system.
More than half of the tools (n = 24; 63.2%) were designed for general health and self-care assessment, indicating a broad focus on overall well-being. The remaining tools (n = 14; 36.8%) were tailored for specific populations, including elderly patients, in-patients, individuals with chronic illnesses or disabilities, and those with psychiatric disorders. This specialization reflects the diverse needs and contexts in which self care assessment is applied.
Tool Length, Data Collection, and Scoring Systems
The length of the identified self care assessment tools varied considerably, ranging from a concise five items in the EQ-5D to a comprehensive 121 items in the SFS. The average number of items per tool was 34.4, suggesting a trend towards moderately detailed assessments. Data collection methods also showed diversity. Eleven tools (28.9%) required staff or individuals familiar with the respondent to record data, often utilizing observation-based methods. A larger proportion, 20 tools (52.6%), were designed for self-administration, emphasizing patient-reported outcomes. Six tools (15.8%) offered versions adaptable to various administration methods, increasing their flexibility in different settings. One tool (SCHDE) did not specify an administration method in the reviewed literature.
Scoring systems for the self care assessment tools were predominantly numerical, with 36 tools (94.7%) using integer rating scales. These scales typically summed item scores to generate a final score reflecting an individual’s self-care ability. The possible score ranges varied widely, from 0 to 410 points, depending on the tool. Interpretation of scores also differed: 26 tools (68.4%) interpreted higher scores as indicating better self-care capability, while four (10.8%) associated higher scores with poorer self-care practices or adherence. For eight tools (21.6%), the scoring direction could not be determined from the available literature.
Completion Time, Reliability, and Validity
Information on the time required to complete the self care assessment tools was reported for only 14 tools (36.8%). For the remaining tools, completion time was estimated based on item count, resulting in an average estimated completion time of 12.8 minutes, with a range from 1.5 to 30 minutes across all 38 tools. This variability in completion time is an important factor to consider when selecting a self care assessment tool for practical application.
Assessments of reliability and validity, crucial indicators of a tool’s psychometric quality, were frequently reported. Thirty-six tools (94.7%) had published studies confirming their validity, and 35 tools (92.1%) had studies confirming reliability. This high prevalence of psychometric testing underscores the commitment to developing robust and scientifically sound self care assessment tools.
Theoretical Underpinnings of Self Care Assessment Tools
The theoretical frameworks underpinning the self care assessment tools varied. Orem’s Theory of Self-Care was explicitly cited as the theoretical basis for eight tools (21.1%). However, a significant number of tools, 14 (36.8%), did not explicitly reference a specific theoretical framework, suggesting a more pragmatic or empirically driven development approach. The remaining tools (47.4%) drew upon a range of theoretical underpinnings, including the Self-Care of Chronic Illness Theory, Item Response Theory, Pender’s Health Promotion Model, Self-efficacy theory, Pörn’s theory of health and adaptedness, The General Health Policy Model, Consumer-driven health care & Chronic Illness Care Model, Middle-range theory of self-care in home-dwelling elderly, Attuned representational model of self, Middle Range Theory of Self-Care of Chronic Illness, the Seven Pillars of Self-Care framework, activation theory, and resilience theory. This diverse range of theoretical foundations reflects the multifaceted nature of self-care and the varying perspectives informing the development of self care assessment tools.
Tool Aims and Administration Trends Over Time
Analysis of the aims of the self care assessment tools revealed a temporal shift in focus. Historically, self-care assessment was primarily geared towards chronic disease management and rehabilitation. However, a notable shift towards prevention-focused tools occurred in the late 1980s, mirroring a broader trend in healthcare towards proactive health promotion. Currently, 17 tools (44.7%) are prevention-focused, nine (23.7%) are rehabilitation-focused, nine (23.7%) target self-management, and a smaller number address both prevention and management or health management and promotion.
Concurrently, the preferred method of administration has evolved. Older tools predominantly relied on observer and interview-style methods, while newer tools increasingly favor self-reported data collection. This transition, evident from the late 1970s to early 1980s, reflects a growing emphasis on patient autonomy and the value of individual perspectives in self care assessment.
Content Assessment: Alignment with the Seven Pillars of Self-Care Framework
The content assessment, utilizing the 7PSC framework, revealed the extent to which each self care assessment tool addressed the seven pillars of self-care. Out of the 38 identified tools, 36 were accessible for content assessment. The configuration matrix (Table 3) summarizes the alignment of each tool with the 7PSC framework.
Overall, the number of pillars addressed by individual self care assessment tools ranged from one to all seven, with an average of 4.6 pillars covered per tool. The most frequently addressed pillars were physical activity, mental wellbeing, and knowledge and health literacy. Pillars related to risk avoidance and the rational use of products and services were less commonly represented across the tools. Specifically, physical activity was addressed by 91.7% of tools, mental wellbeing by 77.8%, knowledge and health literacy by 69.4%, risk avoidance by 66.7%, good hygiene and rational use of products by 52.8% each, and healthy eating by 50%.
Notably, only five self care assessment tools (Rapid Disability Rating Scale, Functional Status Rating System, Appraisal of Self-Care Agency Scale–version A, Lorensen’s Self-care Capability Scale, and Self-Care Inventory – Patient Version) included questions relevant to all seven pillars of self-care. This finding highlights a potential gap in comprehensiveness for many existing self care assessment tools, suggesting room for improvement in capturing the full spectrum of self-care practices.
Discussion: Trends, Gaps, and Future Directions in Self Care Assessment
This scoping review, to our knowledge the first of its kind, provides a comprehensive characterization and mapping of non-mono-disease-specific self care assessment tools for adults. The review highlights key trends in tool development, identifies gaps in content coverage, and suggests future directions for research and practice in the field of self-care assessment.
Evolving Trends in Psychometric Tool Development
The review reveals a significant shift in the focus of self care assessment from chronic disease management and rehabilitation towards prevention. This evolution reflects a growing recognition of individual responsibility in health and a move away from a passive recipient model of healthcare. The rise of the “lifestyle medicine” movement, emphasizing proactive engagement in health and well-being, further reinforces this trend. As healthcare systems grapple with sustainability challenges, the focus on prevention and health maintenance through self-care becomes increasingly critical.
Another key trend is the transition from observer-reported to self-reported data collection methods in self care assessment tools. Newer tools predominantly utilize self-reporting, empowering individuals to actively participate in assessing their own self-care abilities. This shift aligns with patient-centered care approaches and offers benefits such as increased individual engagement and reduced reliance on direct healthcare professional interaction for assessment. However, to mitigate potential biases associated with self-reporting, some tools incorporate mixed methods, combining observer input with self-reported data. This blended approach provides a more comprehensive understanding of self-care behaviors by integrating objective observations with subjective individual experiences. The future of self care assessment may increasingly favor mixed-methods approaches, particularly for informing self-driven healthcare solutions and targeted interventions post-discharge or during rehabilitation.
Emphasis on Self-Care Pillars and Areas for Improvement
The 7PSC framework served as a valuable lens for analyzing the content coverage of self care assessment tools. The analysis revealed chronological trends, particularly since the late 1990s, with increasing emphasis on assessing “knowledge and health literacy,” “risk avoidance,” and the “responsible use of products and services” pillars. This shift likely reflects the growing importance of patient-centered care and the increasing accessibility of online health information.
Despite the growing recognition of health literacy as a crucial determinant of health outcomes, it was one of the less comprehensively addressed pillars in the reviewed self care assessment tools. While numerous validated health literacy tools already exist, the relatively limited integration of health literacy within general self-care assessments suggests an area for potential improvement.
Interestingly, good hygiene, a foundational principle of public health, also appeared to be underrepresented in newer self care assessment tools. The historical success of public health campaigns in promoting hygiene practices may have led to a reduced focus on this pillar in contemporary self-care assessments. However, the ongoing importance of hygiene for preventing infectious diseases and promoting overall well-being warrants renewed attention. Furthermore, the concept of hygiene needs to evolve to encompass contemporary challenges, such as digital hygiene practices in the digital age.
The overall findings suggest that while existing self care assessment tools address many key aspects of health and well-being, there are areas for improvement, particularly regarding comprehensiveness across all seven pillars of self-care. The limited number of tools addressing all seven pillars underscores the need for more holistic approaches to self-care monitoring and evaluation. This is especially relevant in the context of global health initiatives like the UN Sustainable Development Goal 3, aiming to ensure healthy lives and promote well-being for all. Comprehensive self care assessment across all seven pillars could also support healthy aging initiatives and the implementation of the WHO Integrated Care for Older People (ICOPE) framework, which recognizes self-care as a core component for optimizing health outcomes in older adults.
Implications for Research and Practice
The findings of this review have significant implications for future research and practice in self-care. Firstly, there is a clear need for greater consensus on the definition of self-care and the development of a standardized, comprehensive self care assessment tool. Such a tool could be used to evaluate the totality of self-care activities from community, health, and social care perspectives. Standardization would enable more effective evaluation of self-care promotion initiatives and facilitate the identification of areas for improvement.
Secondly, to gain a more complete understanding of health-seeking self-care behaviors, future self care assessment tool development should consider incorporating mixed methods approaches. This would allow researchers to better understand the complex relationship between self-care behaviors and health and social outcomes, and to identify the most effective strategies for promoting self-care across diverse adult populations and settings.
Thirdly, the review highlights the need for more standardized and validated self care assessment tools that cover the full range of self-care practices. Greater consistency in scoring systems, interpretation, and administration methods is also needed to enhance comparability and usability across different contexts. The lack of information on completion time and limited psychometric testing for some tools suggest a need for more rigorous development and validation processes.
Finally, future research should prioritize the development of culturally appropriate self care assessment tools and the validation of existing tools in diverse populations. Considering factors such as diversity, equality, inclusion, language, and digital literacy is crucial to ensure that self care assessment tools are tailored to the specific needs of different populations and are appropriate for the groups they are intended to serve. Routine use of validated, comprehensive self care assessment tools could guide targeted health and social care interventions, enabling policymakers to invest in evidence-based public health initiatives for improved patient and public health outcomes. Ideally, such tools would be self-reported and accessible in various formats (paper or online), while also allowing for interview-style administration when necessary, balancing comprehensiveness with practical resource considerations.
Policy and Practical Implications: Moving Towards Comprehensive Self Care Assessment
Measuring an individual’s self-care capacity and capability is particularly relevant in transitional care settings, such as hospital or rehabilitation discharges. Capacity, in a clinical context, refers to an individual’s decision-making ability, and individuals with self-care capacity are aware of their needs and how to meet them.
Future research should further explore mixed methods approaches and consider cultural and socioeconomic factors in the development of self care assessment tools. The ideal tool for measuring self-care would be a comprehensive, validated, and standardized instrument that encompasses all aspects of the 7PSC framework. It would feature clear and consistent scoring, interpretation, and administration methods, be easy to complete, and possess robust psychometric properties, including reliability and validity, along with clear information on completion time. A key priority is the creation and validation of a modular self care assessment tool that accounts for all seven pillars of self-care, with a clear and consistent scoring system and user-friendly administration.
Recognizing this need, researchers are actively developing the Self-Care CAPabiIity AssessmeNt (CAPITAN) Toolkit. CAPITAN is grounded in the 7PSC framework and the Self-Care Matrix, a unifying framework for self-care. The formative CAPITAN tool includes items relevant to the 7PSC, as well as additional items assessing patient activation, digital literacy, and psychosocial aspects of self-care, including social connectedness. These additional factors are crucial as they significantly influence an individual’s capacity to engage in self-care and interact effectively with community, health, and social care systems. To maximize usability and impact, future self care assessment tools, including CAPITAN, should be designed for inclusivity, translated into multiple languages, and made accessible to diverse populations, demographics, and individuals with specific health conditions.
Strengths and Limitations of the Review
This review’s strength lies in its pragmatic scoping approach, utilizing broad inclusion criteria and search strategies to map the diverse landscape of self care assessment tools. The inclusion of a representative sample of tools developed over seven decades provides valuable insights into the evolution and trends in self-care measurement. The use of the 7PSC framework to analyze content coverage is another key strength, enabling a systematic comparison of tool domains.
Limitations include the non-use of formal quality assessment frameworks like COSMIN for detailed psychometric evaluation of the identified tools, which was deemed beyond the scope of a scoping review. The exclusion of tools for children and adolescents and the restriction to English-language publications are also limitations. Furthermore, the subjective nature of the content assessment using the 7PSC framework introduces potential bias, although this was mitigated through paired assessments and detailed item listing for verification.
Conclusion: Towards Comprehensive and Standardized Self Care Assessment
Positive health behaviors and consistent self-care practices are essential goals for health systems worldwide. This systematic scoping review emphasizes the critical need for a comprehensive and unifying framework to guide the design and assessment of self care assessment tools. Given the increasing importance of self-care monitoring and evaluation in promoting individual and population health, future research should prioritize the development of a comprehensive self care assessment tool that assesses individual capability across all seven pillars of self-care. Such a tool would facilitate routine assessments of self-care capability and inform the delivery of targeted health and social care interventions for adult populations, ultimately contributing to improved health and well-being outcomes.