Depression stands as a widespread mental health disorder across the United States, significantly impacting adults. Recognizing the critical need for early intervention, the U.S. Preventive Services Task Force (USPSTF) advocates for routine depression screening for adults within primary care settings, coupled with evidence-based treatment protocols. This article delves into the crucial role of screening tools in primary care for depression, drawing insights from a quality improvement project that implemented VitalSign6, a measurement-based care program, in an academic medical center to enhance depression screening and treatment.
The Critical Need for Depression Screening in Primary Care
Depression is not just a fleeting feeling of sadness; it is a serious medical condition affecting millions. In the U.S., over 17 million adults experience at least one major depressive episode, representing a significant 7.1% of the adult population. This disorder is not only prevalent but also carries substantial economic and social costs. Estimates place the annual burden of depression at around $210 billion, encompassing medical expenses and lost productivity. Beyond the financial toll, untreated depression leads to profound emotional distress, diminished productivity, strained relationships, and an elevated risk of comorbid conditions. The intricate connection between mental and physical well-being further underscores the urgency of addressing depression, especially as it frequently co-occurs with serious chronic illnesses.
Primary care settings are ideally positioned for the early detection and intervention of depression. A robust body of research supports the integration of depression screening and treatment within these settings. The USPSTF guidelines strongly recommend depression screening for adults aged 18 and older, emphasizing the importance of combining screening with robust support systems and evidence-based approaches. These recommendations are further endorsed by organizations like the American Academy of Family Physicians, highlighting a consensus on the importance of proactive depression management in primary care. Moreover, value-based payment models from Centers for Medicare & Medicaid Services (CMS) are increasingly incentivizing depression screening and follow-up care, making it a quality performance benchmark for accountable care organizations.
Landmark studies, such as the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, have provided compelling evidence for the effectiveness of depression care in primary care settings. This large-scale, multi-site trial demonstrated that treatment outcomes for depression in primary care are comparable to those in specialty care. Despite this strong evidence and national guidelines, a significant gap persists: over half of primary care patients with depression remain undiagnosed and undertreated. National data reveals alarmingly low depression screening rates in primary care visits, highlighting a critical need for improved implementation of effective screening strategies.
Efforts to bridge this gap are increasingly focused on the adoption of standardized screening tools in primary care. These tools are designed for quick and efficient identification of individuals who may be experiencing depression, enabling timely intervention and improved patient outcomes.
Common Screening Tools for Depression in Primary Care
Among the various tools available, the Patient Health Questionnaire (PHQ)-2 and PHQ-9 stand out as the most widely utilized and validated depression screening instruments for adults. These tools are recognized for their clinical utility and diagnostic accuracy in primary care settings.
The PHQ-2: This two-item questionnaire serves as an initial screening step. It focuses on the core symptoms of depression: depressed mood and anhedonia (loss of interest or pleasure). Patients rate the frequency of these symptoms over the past two weeks on a scale from 0 (“not at all”) to 3 (“nearly every day”). A total score of 3 or higher is considered a positive screen, indicating the need for further assessment. The PHQ-2 is designed to be highly sensitive, meaning it is effective at identifying most individuals who have depression, and also demonstrates good specificity, correctly identifying those who are unlikely to have depression.
The PHQ-9: If a patient screens positive on the PHQ-2, or if there is clinical suspicion of depression, the PHQ-9 is administered. This more comprehensive, nine-item questionnaire is directly based on the DSM-5 criteria for major depressive disorder. It delves deeper into the severity of depressive symptoms, assessing each of the nine diagnostic criteria. Scores on the PHQ-9 range from 0 to 27, with score ranges corresponding to different levels of depression severity: minimal, mild, moderate, moderately severe, and severe. The PHQ-9 not only aids in diagnosing depression but also serves as a valuable tool for monitoring symptom severity over time and tracking treatment response.
Both the PHQ-2 and PHQ-9 have been rigorously validated in primary care populations. Meta-analyses have confirmed their effectiveness, validity, and reliability in detecting depression in this setting. Their brevity and ease of administration make them practical tools for busy primary care clinics, facilitating routine screening without placing undue burden on clinicians or patients.
Implementing Screening Tools and Measurement-Based Care
While screening tools are essential, their impact is maximized when integrated within a system of care that includes standardized treatment protocols and referral pathways. Measurement-based care (MBC) offers such a comprehensive framework. MBC utilizes validated screening tools, standard symptom measurements, and evidence-based decision support to guide primary care physicians in the diagnosis, treatment, follow-up, and referral of patients with depression.
The VitalSign6 program exemplifies an MBC approach. Developed by The University of Texas Southwestern Medical Center for Depression Research and Clinical Care (CDRCC), VitalSign6 is a web-based program designed to seamlessly integrate depression screening and management into the primary care workflow. It leverages the PHQ-2 and PHQ-9, along with other measures, to provide clinicians with real-time data and clinical decision support.
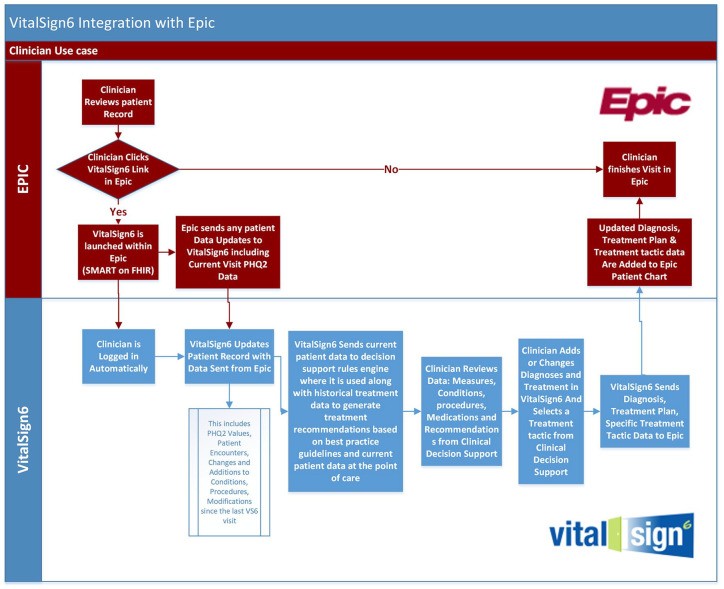
The implementation of VitalSign6 in a primary care clinic within an academic medical center demonstrated the practical application and benefits of MBC. The project aimed to improve depression identification and management by embedding VitalSign6 within the clinic’s electronic health record (EHR) system. This integration was achieved through an application programming interface (API) that allowed VitalSign6 to interoperate with the EHR, Epic.
Key aspects of the VitalSign6 implementation included:
- EHR Integration: The seamless integration with Epic allowed for efficient data flow and clinician access to screening results and decision support tools directly within their familiar EHR environment.
- Workflow Integration: VitalSign6 was designed to fit within the existing clinic workflow. Patients completed self-reported measures on tablets during check-in, and results were immediately available to providers.
- Clinical Decision Support (CDS): The program provided evidence-based treatment recommendations and decision support tools to aid physicians in tailoring treatment plans.
- Training and Support: Comprehensive training was provided to physicians and staff on depression, MBC, and the use of VitalSign6. On-site support was also available during the initial implementation phase.
The results of the VitalSign6 project were encouraging. Screening rates significantly improved, with over 95% of patients being screened for depression. A substantial proportion of patients who screened positive were diagnosed and initiated on measurement-based care. Furthermore, patients receiving MBC showed a statistically significant decrease in self-reported depression scores from baseline to follow-up. The project demonstrated the feasibility and effectiveness of using MBC programs like VitalSign6 to enhance depression care in primary care settings.
Addressing Challenges and Optimizing Implementation
Despite the positive outcomes, the VitalSign6 project also highlighted challenges in implementing new technologies and workflows in busy primary care clinics. Physician and staff surveys revealed concerns about workflow disruption and technical issues related to EHR interoperability. Specifically, the initial implementation required the use of Epic Welcome tablets for PHQ-2 administration, which was a new workflow for the clinic and contributed to some initial resistance and technical hiccups. Physicians also reported difficulties with data transfer and system usability.
These challenges underscore the importance of careful planning and attention to workflow integration when implementing depression screening programs. Key strategies for successful implementation include:
- Workflow Optimization: Thoroughly assess existing clinic workflows and design screening processes that minimize disruption and integrate seamlessly.
- Technical Support and Training: Provide robust technical support and comprehensive training to all staff members to ensure smooth adoption and utilization of new technologies.
- User-Friendly Technology: Prioritize user-friendly technology solutions that are intuitive and easy to use for both clinicians and patients. Address interoperability issues proactively to ensure seamless data exchange between systems.
- Stakeholder Engagement: Engage physicians and staff in the implementation process, solicit their feedback, and address their concerns to foster buy-in and ownership.
Addressing these challenges is crucial for the widespread and sustainable adoption of depression screening programs in primary care. By optimizing implementation strategies and leveraging technology effectively, primary care settings can significantly improve the identification and management of depression, leading to better outcomes for patients.
Conclusion: Enhancing Depression Care Through Effective Screening
Depression screening in primary care is not just recommended; it is essential for improving the health and well-being of adults. Validated screening tools like the PHQ-2 and PHQ-9 provide primary care clinicians with practical and effective means to identify individuals who may be struggling with depression. When implemented within a comprehensive system of care, such as measurement-based care, these tools can significantly enhance the quality of depression care, leading to improved patient outcomes, including symptom reduction and remission.
While challenges exist in implementing new screening programs and technologies, the potential benefits are substantial. By prioritizing workflow optimization, providing adequate training and support, and leveraging user-friendly, interoperable technologies, primary care settings can overcome these hurdles and effectively integrate depression screening into routine practice. Continued efforts to refine implementation strategies and expand access to measurement-based care programs are crucial for ensuring that all individuals receive the timely and effective depression care they need within the primary care setting.