I. Introduction to the PUSH Tool and Diabetic Foot Ulcers
Diabetic foot ulcers (DFUs) are a significant complication of diabetes mellitus, affecting a large percentage of diabetic individuals throughout their lives. These chronic wounds pose substantial health risks, often leading to severe outcomes like amputation. Effective DFU management is crucial, requiring a multifaceted approach including off-loading, debridement, infection control, and advanced wound care techniques. Central to this management is the ability to accurately monitor wound healing and predict healing time, allowing clinicians to assess treatment effectiveness and intervene promptly when healing is delayed.
Traditional methods for monitoring DFU healing have included tracking changes in wound area. While effective, these methods can be time-consuming and may not provide immediate insights into healing progress. The Pressure Ulcer Scale for Healing (PUSH) tool, developed by the National Pressure Ulcer Advisory Panel (NPUAP), offers a clinically efficient approach for monitoring wound healing. Originally validated for pressure and venous ulcers, the PUSH tool’s utility in evaluating DFUs has remained less explored. Furthermore, the quantitative trajectory of PUSH scores during DFU healing and its potential for predicting time-to-heal have not been fully elucidated.
This study delves into the predictive validity of the PUSH tool (version 3.0) for neuropathic DFUs. We investigated the pattern of PUSH scores over time in healing DFUs, assessed the PUSH tool’s ability to predict DFU healing time, and identified which components of the PUSH tool—wound size, exudate amount, or tissue type—are most influential in predicting healing duration. The goal is to provide clinicians with a practical tool to enhance DFU management and improve patient outcomes.
II. Understanding the PUSH Tool and its Components
The PUSH tool (version 3.0) is a structured assessment instrument designed to monitor the healing status of wounds. It comprises three key parameters, each scored independently and then summed to produce a total PUSH score. This score ranges from 0 to 17, with a score of 0 indicating a completely healed wound. The three components are:
-
Length × Width (Size): This is determined by measuring the longest length and widest width of the wound in centimeters and multiplying these values to estimate the wound surface area in square centimeters. The resulting area is then categorized on a scale from 0 to 10, where 0 represents a healed wound and 10 corresponds to a wound area greater than 24 cm². Wound size is a critical indicator of healing progress, with a reduction in size generally signifying positive healing.
-
Exudate Amount: Wound exudate, the fluid that leaks from a wound, provides insights into the wound environment and healing stage. The PUSH tool assesses exudate amount on a scale of 0 to 3: 0 for none, 1 for light, 2 for moderate, and 3 for heavy exudate. Changes in exudate volume can reflect infection status or healing progression.
-
Tissue Type: The type of tissue present in the wound bed is a crucial indicator of healing. The PUSH tool categorizes tissue type on a scale from 0 to 4: 0 for closed (healed), 1 for epithelial tissue (new skin), 2 for granulation tissue (healthy healing tissue), 3 for slough (yellow/white dead tissue), and 4 for necrotic tissue (black, dead tissue). A shift from necrotic tissue or slough towards granulation and epithelial tissue is a positive sign of wound healing.
Figure 1: Visual representation of PUSH tool components and their role in wound assessment, highlighting Length x Width measurement, Exudate Amount evaluation, and Tissue Type classification for effective wound monitoring.
Regular assessment using the PUSH tool enables healthcare providers to quantitatively track changes in these wound characteristics, providing a standardized method to monitor healing trends and adjust treatment plans as needed.
III. Study Methodology: Evaluating PUSH Tool in Diabetic Foot Ulcer Healing
This study employed a prospective, descriptive design to evaluate the PUSH tool’s effectiveness in monitoring the healing of neuropathic DFUs. A group of 18 patients with Wagner grade 2 or higher neuropathic, non-ischemic foot ulcers were monitored over a 13-week period. Ulcers were located on the plantar surface of the foot and were confirmed to be non-ischemic through toe pressure measurements.
Standardized Wound Care Protocol
All participants received standardized DFU treatment, including moist wound dressings and regular debridement, ensuring consistency in care across the study group. This controlled environment allowed for a focused evaluation of the PUSH tool’s predictive capabilities without variations introduced by differing treatment regimens.
PUSH Assessment and Healing Criteria
Trained research staff assessed each study ulcer using the PUSH tool every two weeks. To ensure reliability, inter-rater reliability was assessed and confirmed to be high across all PUSH components. Healing was defined as complete re-epithelialization of the wound bed, confirmed through visual inspection. Data collection included patient demographics such as age, gender, race, diabetes type, and ulcer location. Wound size was measured using digital imaging and VevMD software for accuracy.
Data Analysis: Trajectory and Predictive Modeling
The study focused on DFUs that healed within the 13-week follow-up, allowing for modeling of PUSH score trajectories from initial assessment to complete healing. Piecewise linear regression models were used to analyze:
- PUSH Score Trajectory: To understand how PUSH scores change over time in healing DFUs.
- PUSH as a Predictor of Time-to-Heal: To determine if initial PUSH scores could predict the duration of healing.
- Contribution of PUSH Sub-items: To identify which individual components of the PUSH tool (size, exudate, tissue type) were most predictive of healing time.
By employing these statistical methods, the study aimed to rigorously evaluate the PUSH tool’s utility in the context of neuropathic DFU management.
IV. Key Findings: PUSH Tool Effectively Monitors and Predicts DFU Healing
The study yielded significant findings regarding the PUSH tool’s application in monitoring and predicting the healing of neuropathic DFUs.
PUSH Scores Decrease Significantly During DFU Healing
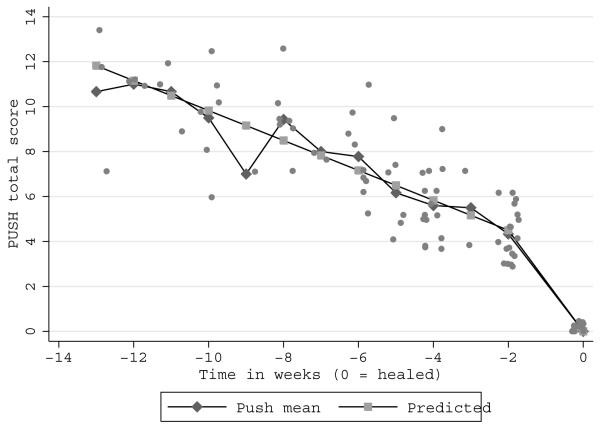
The analysis revealed a significant decrease in PUSH scores over time in healing DFUs. The trajectory of PUSH scores was well-represented by a piecewise linear regression model, showing a two-phase healing pattern. Initially, PUSH scores decreased at a rate of 0.67 points per week. Notably, in the two weeks immediately preceding complete healing, the rate of decrease accelerated to 2.25 points per week. This accelerated decrease in PUSH scores in the final stages of healing highlights the tool’s sensitivity to changes as the wound nears closure.
Figure 2: Graphical depiction of PUSH score trajectory over time, illustrating the piecewise linear model and the accelerated decrease in scores as DFUs approach complete healing, showcasing the PUSH tool’s dynamic tracking of wound improvement.
PUSH Tool Effectively Predicts Time-to-Heal for DFUs
The study demonstrated that the PUSH tool is a valuable predictor of DFU healing time. Statistical models showed a significant correlation between initial PUSH scores and the time required for complete healing. For instance, a DFU with an initial PUSH score of 10 was predicted to heal in approximately 8.8 weeks, while a DFU with a score of 4 was expected to heal in about 2.6 weeks. This predictive capability enables clinicians to set realistic healing expectations and identify DFUs that are not progressing as anticipated.
Wound Size (Length × Width) is the Most Predictive PUSH Component
Interestingly, when examining the individual components of the PUSH tool, wound size (length × width) emerged as the most significant predictor of healing time. In fact, wound size alone was found to be as effective as the total PUSH score in predicting healing duration. While exudate and tissue type are important for comprehensive wound assessment, they were not as strongly correlated with healing time in this study as wound size. This suggests that in resource-limited settings or when seeking a simplified assessment, wound size measurement alone can provide valuable prognostic information.
Figure 3: Visual representation of time-to-heal prediction based on DFU Length x Width, demonstrating the effectiveness of size measurement as a key indicator for prognosis and simplified wound assessment in clinical settings.
These findings collectively underscore the PUSH tool’s utility in DFU management, particularly its ability to monitor healing progress and predict healing time, with wound size being a surprisingly robust predictor on its own.
V. Clinical Implications and Conclusion: Simplifying DFU Wound Care with the PUSH Tool
This study provides compelling evidence for the use of the PUSH tool as a valuable asset in the clinical management of neuropathic DFUs. The tool’s ability to effectively track healing progress and predict time-to-heal offers several key clinical advantages:
- Early Identification of Delayed Healing: By predicting expected healing times based on PUSH scores, clinicians can promptly identify DFUs that are not healing as anticipated. This allows for timely intervention, including re-evaluation of treatment strategies and consideration of advanced wound care modalities.
- Objective Monitoring of Treatment Effectiveness: Regular PUSH assessments provide a standardized, objective measure of wound healing progress. This enables healthcare providers to quantitatively evaluate the effectiveness of current treatments and make data-driven decisions regarding adjustments to care plans.
- Simplified Wound Assessment: The finding that wound size alone is a strong predictor of healing time highlights the potential for simplified wound assessments. In busy clinical settings, focusing on accurate wound size measurement can provide significant prognostic information, streamlining the assessment process without sacrificing valuable insights.
- Resource Allocation and Patient Management: Predicting healing time can aid in resource allocation, allowing clinics to prioritize patients with slower-healing wounds for more intensive management. It also helps in setting realistic patient expectations regarding the duration of treatment and recovery.
Conclusion
In conclusion, this research demonstrates that the PUSH tool is a reliable and effective instrument for monitoring healing and predicting time-to-heal in neuropathic diabetic foot ulcers. The tool’s ease of use, coupled with its predictive capabilities, makes it a valuable addition to the wound care clinician’s toolkit. While the full PUSH assessment provides a comprehensive wound profile, the study’s finding that wound size is a key predictor offers opportunities for simplified assessment protocols. Integrating the PUSH tool into routine DFU care can enhance clinical decision-making, improve patient outcomes, and streamline wound management processes. For wound care specialists seeking effective and efficient tools, the PUSH tool stands out as a significant advancement in diabetic foot ulcer management.