Introduction
Accurate prognosis is crucial in palliative care, guiding end-of-life decisions and aligning patient expectations with realistic outcomes. Patients often hold overly optimistic views about their prognosis, while expressing a desire for honest and accurate survival estimates from their physicians [6, 7]. Clinician predictions, although generally more accurate than patient self-assessments [1, 5], still exhibit inaccuracies [8, 9]. This has led to recommendations for clinicians to augment their judgment with validated prognostic algorithms [10, 11]. Several prognostic tools have been developed for advanced cancer patients in palliative care settings [12, 13], but few have been rigorously compared against clinicians’ own survival predictions [14–18].
The Prognosis in Palliative Care Study (PiPS) previously developed and validated prognostic tools (PiPS-A and PiPS-B) for 14-day and 56-day survival in palliative cancer care [19]. These tools categorize patients into risk groups (days, weeks, or years) and have shown comparable accuracy to multi-professional clinical survival estimates [19, 21]. The PiPS2 study further validated PiPS and evaluated other prognostic models including the Palliative Prognostic Index (PPI) [22], Palliative Performance Scale (PPS) [23], Palliative Prognostic (PaP) score [24], and Feliu Prognostic Nomogram (FPN) [25]. Some tools like PPI and PPS do not require blood tests, similar to PiPS-A, while PaP and FPN, like PiPS-B, do. This study focuses on evaluating PaP, FPN, PPI, and PPS in advanced cancer patients and comparing their prognostic performance against clinical predictions of survival (CPS).
Methods
This multi-center, prospective cohort validation study, registered as ISRCTN 13688211 [20], was approved by the Yorkshire and Humber-Leeds East Research Ethics Committee (16/YH/0132). The study protocol is publicly available [20].
Participants
Patients were recruited from 27 palliative care services across the UK, including community, hospital, and inpatient palliative care units. Participants were adults with advanced cancer referred to palliative care, with or without the capacity to consent. Capacity assessment was performed by the Principal Investigator or delegate at each site [26]. Informed consent was obtained from patients with capacity, while a personal or nominated consultee provided advice for patients without capacity.
Inclusion and Exclusion Criteria
Inclusion criteria were: (1) incurable cancer, (2) age 18 years or older, (3) recent referral to palliative care services, and (4) for patients with capacity, ability to understand the Patient Information Sheet or consultee approval for those without capacity. The exclusion criterion was treatment with curative intent.
Data Collection
Baseline prognostic data were collected from medical notes, clinical staff discussions, and patient interviews. Data required for each prognostic score are detailed in Table 1. Additional data for PiPS scores were collected but are reported separately [21].
Table 1. Variables Required for Prognostic Score Calculation.
| Variable Type | Variable Name | PaP | FPN | PPI | PPS |
|---|---|---|---|---|---|
| Clinician Assessments | Clinician Prediction of survival | x | |||
| Eastern Cooperative Oncology Group | x | ||||
| Karnofsky Performance Scale | x | ||||
| Palliative Performance Scale (PPS) | x | x | |||
| Time to terminal disease | x | ||||
| Blood Tests | Albumin | x | x | ||
| Lactate Dehydrogenase | x | ||||
| Lymphocyte count | x | x | x | ||
| White blood count | x | x | |||
| Clinical Signs & Symptoms | Anorexia | x | x | ||
| Delirium | x | x | |||
| Dyspnoea at rest | x | x | x | ||
| Oedema | x | x | |||
| Oral intake | x | x |
Prognostic Tools
- Palliative Prognostic (PaP) score: Categorizes patients into three risk groups based on 30-day survival probability: <30%, 30-70%, and >70%. Higher scores indicate poorer prognosis. PaP uses clinician prediction, Karnofsky performance status, anorexia, dyspnoea, white blood cell count, and lymphocyte percentage.
- Feliu Prognostic Nomogram (FPN): Predicts 15, 30, and 60-day survival probability using ECOG performance status [27], serum albumin, Lactate Dehydrogenase, lymphocyte count, and time from initial diagnosis to terminal disease diagnosis.
- Palliative Performance Scale (PPS): Assesses functional status in palliative care, ranging from 10% (lowest function) to 100% (highest function). Scored by healthcare professionals.
- Palliative Prognostic Index (PPI): Stratifies patients into three survival groups: <3 weeks (score >6), <6 weeks (score >4), and >6 weeks (score ≤4) based on PPS, oral intake, dyspnoea, oedema, and delirium.
Clinical Prediction of Survival (CPS)
Attending doctors and nurses independently estimated patient survival. Doctor predictions were prioritized, with nurse predictions used when doctor data was unavailable. Clinicians provided estimates in various formats: approximate survival (days, weeks, months+), specific weeks (up to 12 weeks), and survival probabilities at 1, 3, 7, 15, 30, and 60 days. Clinician demographics were collected but individual clinicians were not identified.
Survival Outcome
Death dates were obtained from NHS Digital (https://digital.nhs.uk/) at least three months post-recruitment.
Statistical Analysis
The primary outcome was patient survival from enrollment, compared against clinician predictions and prognostic scores. Prognostic tool performance was evaluated against actual survival and CPS. Sample size was calculated for PiPS-B validation [21], deemed sufficient for validating other tools (PPI, PPS, PaP, FPN).
Discrimination (distinguishing risk groups) was assessed using C-statistics, Harrell’s C-index, and Kaplan-Meier curves. Calibration (agreement between predicted and observed outcomes) was assessed using calibration slopes and comparing predicted and observed survival proportions at specific time points.
- PaP: Kaplan-Meier curves for risk groups, median survival analysis, and comparison of predicted vs. observed 30-day survival proportions for PaP and CPS. C-statistic calculated using risk group midpoints.
- FPN: Harrell’s C-index, calibration slope, and comparison of FPN and CPS predicted survival probabilities at 15, 30, and 60 days against observed survival.
- PPI: McNemar’s test to compare PPI and CPS prediction accuracy, C-statistics for 3-week and 6-week predictions, and Kaplan-Meier curves for PPI risk groups.
- PPS: Kaplan-Meier curves for PPS levels and CPS predicted 30-day survival probabilities, C-statistic calculated against published 30-day survival probabilities for PPS categories [30].
Results
A total of 1833 participants (1610 with capacity) were enrolled. Median survival from enrollment was 45 days (IQR 16-140). Participant characteristics are detailed in Table 2.
Table 2. Participant Characteristics.
| Variable | |
|---|---|
| Age (years); mean (SD); n = 1832[*] | 70.2 (11.9) |
| Gender; n (%); n = 1832[*] | |
| Male | 938 (51.2) |
| Female | 894 (48.8) |
| Location; n (%) | |
| Inpatient Palliative Care Unit | 1241 (67.7) |
| Community Palliative Care Team | 468 (25.5) |
| Hospital Palliative Care Team | 124 (6.8) |
| Site of Primary tumour[**]; n (%) | |
| Lung | 362 (19.8) |
| Upper GI tract | 337 (18.4) |
| Head and neck | 280 (15.3) |
| Prostate | 160 (8.7) |
| Breast | 146 (8.0) |
| Gynaecological | 133 (7.3) |
| Other | 123 (6.7) |
| Urological (bladder, testes, renal) | 112 (6.1) |
| Lower GI tract | 81 (4.4) |
| Haematological | 70 (3.8) |
| Unknown | 45 (2.5) |
| Neurological | 38 (2.1) |
| Rare tumour | 27 (1.5) |
| Site of metastatic diseases; n (%) | |
| Bone | 555 (30.3) |
| Liver | 538 (29.4) |
| Nodal | 516 (28.2) |
| Lung | 477 (26.0) |
| Other | 353 (19.3) |
| None | 279 (15.2) |
| Brain | 134 (7.3) |
| Pleural effusion | 98 (5.4) |
| Ascites | 95 (5.2) |
| Adrenal | 79 (4.3) |
| Unknown | 60 (3.3) |
| Skin | 36 (2.0) |
| Renal | 20 (1.1) |
| Currently receiving tumour therapy; yes n (%) | 391 (21.3) |
| If yes, type of therapy: | |
| Chemotherapy | 190 (48.6) |
| Radiotherapy | 118 (30.2) |
| Hormone therapy | 76 (19.4) |
| Other tumour directed therapy (e.g. immunotherapy) | 42 (10.7) |
| Capacity to consent; n (%) | 1610 (87.8) |
| Time between diagnosis and date became incurable; n = 1821 | |
| Mean (SD); months | 13.2 (32.8) |
| Median (IQ Range); months | 0 (0, 12) |
| Abbreviated Mental Test Score (AMTS); n = 1826 | |
| Less than 4 | 208 (11.4) |
| Greater or equal 4 | 1618 (88.6) |
| Presence or absence of key symptoms | |
| Anorexia; yes; n = 1830 | 968 (52.9) |
| Dysphagia; yes; n = 1830 | 554 (30.3) |
| Dyspnoea; yes; n = 1831 | 652 (35.6) |
| Fatigue; yes; n = 1831 | 1617 (88.3) |
| Lost weight; yes; n = 1831 | 1194 (65.2) |
| Clinical assessments | |
| Ascites; n = 1830 | 245 (13.4) |
| Presence of peripheral oedema; n = 1831 | 685 (37.4) |
| Pulse rate; beats/min; mean (SD); n = 1817 | 82.2 (14.7) |
| Presence of delirium; n = 1830 | 66 (3.6) |
| If Yes, is it considered to be caused by a single medication | 2 (3.0) |
| Oral intake; n = 1830 | |
| Normal | 587 (32.1) |
| Moderately reduced | 666 (36.4) |
| Severely reduced | 577 (31.5) |
| Eastern Co-operative Oncology Group score (ECOG) Performance status; n = 1831 | |
| Grade 0 | 15 (0.8) |
| Grade 1 | 202 (11.0) |
| Grade 2 | 520 (28.4) |
| Grade 3 | 822 (44.9) |
| Grade 4 | 272 (14.9) |
| Global health status (overall health); n (%); n = 1823 | |
| 1 (Very poor) | 144 (7.9) |
| 2 | 414 (22.7) |
| 3 | 680 (37.3) |
| 4 | 348 (19.1) |
| 5 | 180 (9.9) |
| 6 | 49 (2.7) |
| 7 (Excellent) | 8 (0.4) |
| Karnofsky Performance Scale (KPS); n (%); n = 1830 | |
| 10 | 63 (3.4) |
| 20 | 108 (5.9) |
| 30 | 136 (7.4) |
| 40 | 229 (12.5) |
| 50 | 465 (25.4) |
| 60 | 404 (22.1) |
| 70 | 276 (15.1) |
| 80 | 114 (6.2) |
| 90 | 33 (1.8) |
| 100 | 2 (0.1) |
| Full blood count | Mean (SD) |
| White blood count (x109/L); n = 1602 | 11.3 (11.2) |
| Lymphocyte count (x109/L); n = 1596 | 1.2 (2.0) |
| Neutrophil count (x109/L); n = 1600 | 8.8 (6.2) |
| Platelets (x109/L); n = 1601 | 312.9 (147.6) |
| Biochemistry | |
| Urea (mmol/L); n = 1601 | 8.0 (6.4) |
| Albumin (g/L); n = 1600 | 30.1 (7.0) |
| Alkaline phosphatase (U/L); n = 1587 | 231.7 (319.9) |
| Alanine transaminase (U/L); n = 1581 | 33.3 (71.7) |
| C reactive protein (mg/L); n = 1565 | 68.6 (73.5) |
| Lactate Dehydrogenase (mmol/L); n = 1467 | 505.4 (446.0) |
Notes for Table 2
[*] One participant preferred not to say.
[**] 73 participants had more than one primary tumour.
Clinician Participant Characteristics
Analysis suggested most doctors were palliative care specialists (86%). Doctors had an average of 12.8 years post-qualification and 6.2 years palliative care experience. Nurses were almost all palliative care specialists (98%) with 19.4 years post-qualification and 8.5 years palliative care experience.
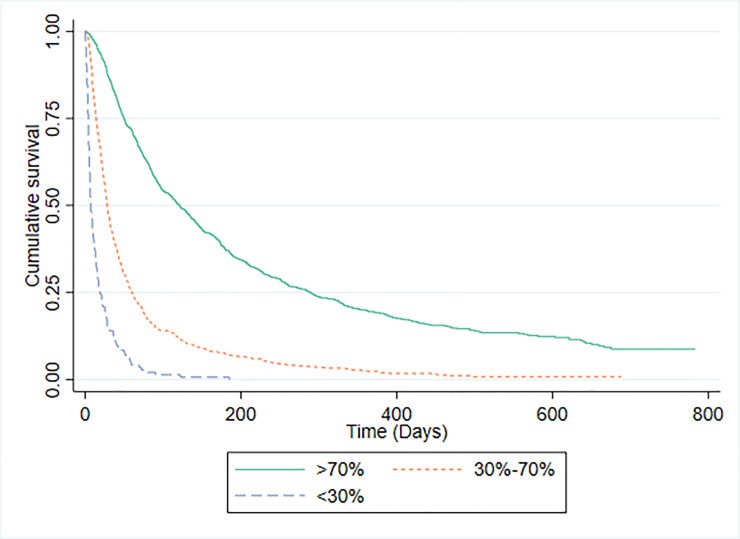
Palliative Prognostic Score (PaP)
PaP scores were available for 1592 patients. The PaP model C-statistic was 0.771 (95% CI 0.749-0.792). Risk group distribution was: Group A (predicted >70% 30-day survival) 49.1%, Group B (30-70%) 41.1%, and Group C (<30%) 9.0%. Median survival for PaP score available patients was 51 days (IQR 21-151). Median survival and observed 30-day survival for each PaP risk group were:
- Group A: 121 days (IQR 49-289), 86.5% 30-day survival.
- Group B: 28 days (IQR 14-60), 46.8% 30-day survival.
- Group C: 7 days (IQR 4-19), 15.4% 30-day survival.
Comparison with CPS risk groups (Figure 2) showed similar stratification:
- CPS Group A: 112 days (IQR 45-272), 85.3% 30-day survival.
- CPS Group B: 30 days (IQR 15-73), 49.3% 30-day survival.
- CPS Group C: 11 days (IQR 5-27), 23.4% 30-day survival.
Fig 1. Kaplan-Meier survival curves for PaP risk groups illustrating survival probability across different risk categories defined by the Palliative Prognostic Score.
Fig 2. Kaplan-Meier survival curves according to CPS risk groups, demonstrating the effectiveness of Clinical Prediction of Survival in stratifying patients by mortality risk.
Feliu Prognostic Nomogram (FPN)
FPN’s Harrell’s C-index was 0.684 (95% CI: 0.669-0.700; n=1432), considered moderately discriminatory. Calibration slope was 1.049 (95% CI: 0.939-1.158), indicating good calibration. Median (IQR) predicted 15-day survival probabilities were similar for FPN [72.0% (62.9-81.0)] and CPS [80% (70-95)], aligning with observed 15-day survival [80.7% (1156/1432)]. 30-day predictions were also similar: FPN 50.3% (37.9-64.3), CPS 70% (50-80), observed 65.1% (932/1432). 60-day predictions: FPN 28.9% (17.3-45.0), CPS 50% (20-70), observed 47.1% (675/1432).
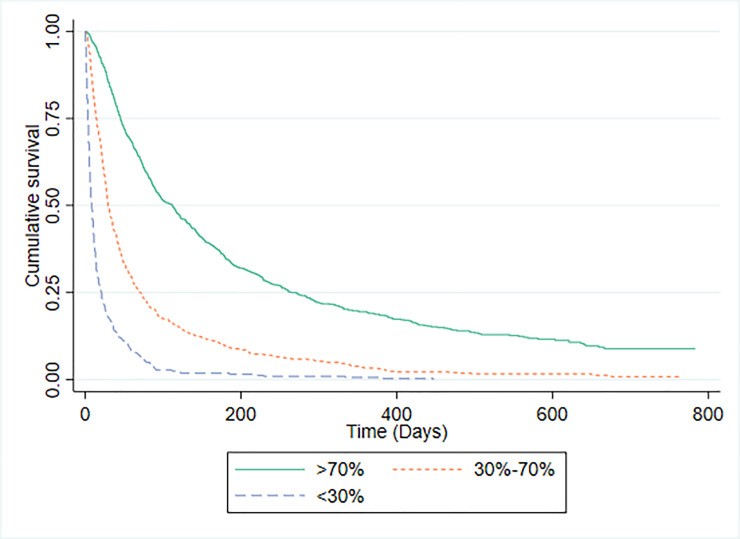
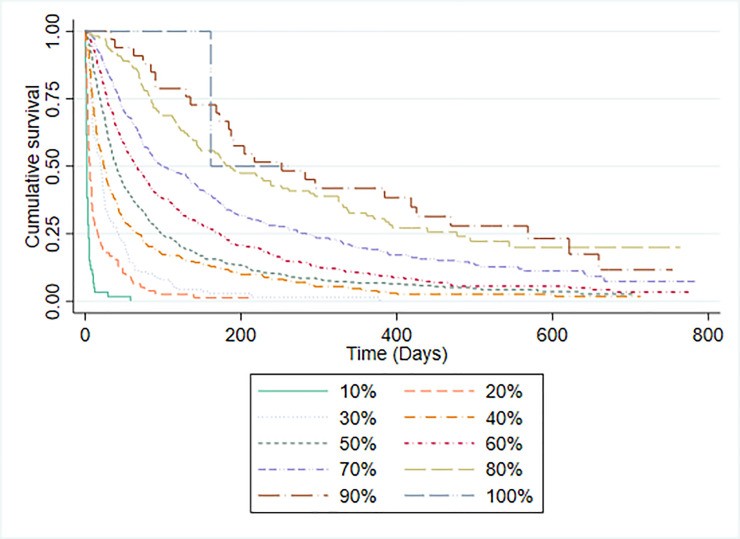
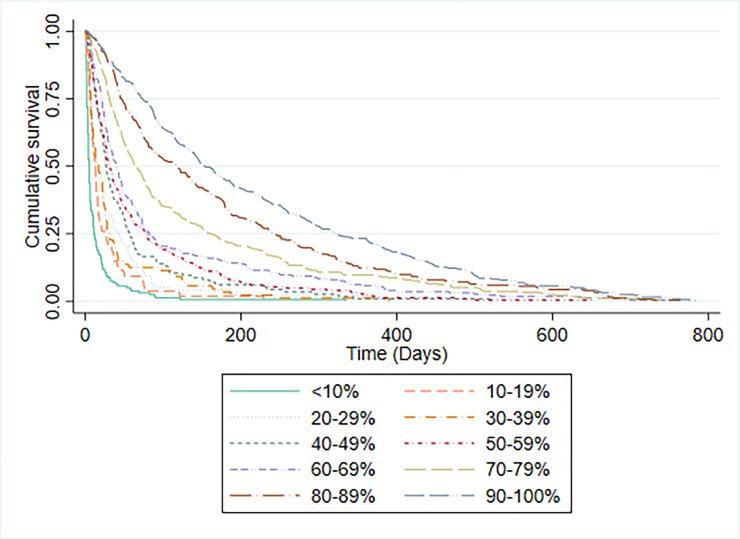
Palliative Performance Scale (PPS)
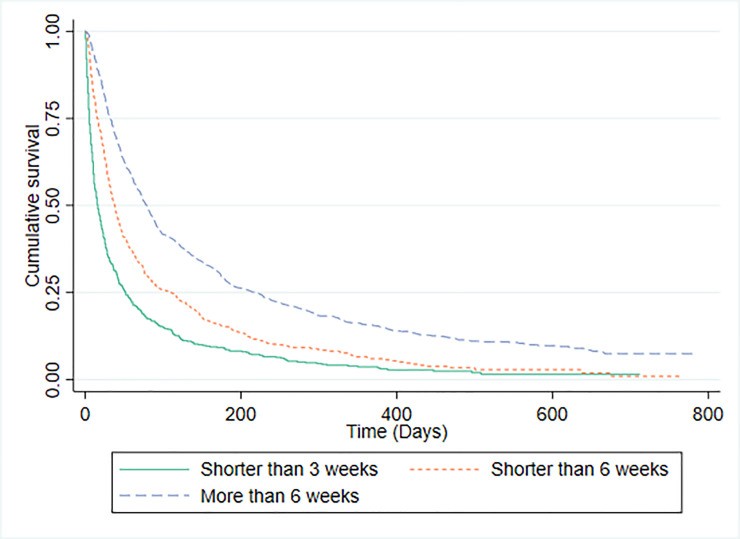
PPS scores and median survival times are in Table 3. PPS C-statistic was 0.757 (95% CI 0.735-0.778). Kaplan-Meier curves (Figure 3) showed increasing median survival with better PPS levels, except for PPS 100% due to participant scarcity. CPS also effectively categorized patients into iso-prognostic groups based on 30-day survival probability (Figure 4), similar to PPS.
Table 3. Participant Number and Median Survival Time by PPS Category, illustrating the correlation between PPS score and patient survival duration in palliative care.
| PPS score | n (%) | Median survival time in days (interquartile range) |
|---|---|---|
| 10% | 60 (3.3) | 2 (1 to 4) |
| 20% | 78 (4.3) | 6 (3 to 16) |
| 30% | 138 (7.6) | 20 (7 to 42) |
| 40% | 273 (14.9) | 24 (10 to 69) |
| 50% | 493 (27.0) | 40 (19 to 97) |
| 60% | 376 (20.6) | 65 (28 to 172) |
| 70% | 265 (14.5) | 99 (44 to 284) |
| 80% | 109 (6) | 186 (85 to 477) |
| 90% | 33 (1.8) | 252 (135 to 568) |
| 100% | 2 (0.1)[*] | – |
[*]too few participants to judge survival times.
Fig 3. Kaplan-Meier survival curves by PPS level, demonstrating the survival distribution across different Palliative Performance Scale levels.
Fig 4. Kaplan-Meier survival curves by 30-day CPS probability, illustrating how Clinical Prediction of Survival effectively stratifies patients based on their 30-day survival likelihood.
Palliative Prognostic Index (PPI)
PPI risk group distribution: >6 score (predicted <3 weeks survival) 49.2%, >4 score (predicted <6 weeks survival) 23.4%, ≤4 score (predicted >6 weeks survival) 49.2%. C-statistics: 3-week prediction 0.675 (0.652-0.699), 6-week prediction 0.655 (0.633-0.676). Median (IQR) survival for PPI risk groups:
- Predicted <3 weeks: 16 days (IQR 2-52).
- Predicted <6 weeks: 38 days (IQR 15-106).
- Predicted >6 weeks: 79 days (IQR 32-219).
Table 4 compares PPI and CPS prediction accuracy against observed survival. CPS correctly predicted outcome in 62.5% of cases, PPI in 54.2%. PPI was significantly less accurate than CPS (p<0.001).
Fig 5. Kaplan-Meier survival curves for PPI predictions, showing survival distributions for Palliative Prognostic Index predicted survival categories.
Table 4. Accuracy Comparison of PPI vs. CPS Predictions Against Observed Deaths, highlighting the comparative performance of Palliative Prognostic Index and Clinical Prediction of Survival.
| Variable | Doctors’ predictions compared to observed deaths |
|---|---|
| PPI predictions compared to observed deaths | CPS was correct |
| PPI prediction was correct | 745 (40.8%) |
| PPI prediction was incorrect | 398 (21.8%) |
| Total | 1143 |
Discussion
This study benchmarked prognostic tools against clinical prediction of survival (CPS), the current standard in palliative care. We found that clinicians were as effective as PaP in categorizing patients by 30-day survival probability and as effective as FPN for 15, 30, and 60-day probabilities. PPI was significantly less accurate than CPS for 3 and 6-week survival predictions. PPS and CPS showed similar abilities in sorting patients into iso-prognostic groups.
Direct comparison between prognostic models and CPS presents methodological challenges [16, 18, 34]. For example, PaP categorizes patients into risk groups with probability ranges rather than specific survival predictions. While PaP effectively distinguished groups with different 30-day survival probabilities (86.5%, 46.8%, 15.4% for Groups A, B, C respectively), clinicians demonstrated equal capability in this regard (85.2%, 49.7%, 17.7%).
Simplifying PaP as a continuous variable facilitates comparison with CPS [18, 34–36], but disregards clinically relevant risk categories [31]. Hui et al. [18] reported a PaP C-index of 0.64, lower than clinician predictions. Mukai et al. [34] found PaP AUC higher than two physicians. However, understanding how risk categories like PaP’s Group B (30-70% 30-day survival probability) translate to clinical utility is crucial. Clinicians, similarly, can identify patients within this probability range using intuition alone. Furthermore, PaP’s probabilistic categories may lack face validity and practical utility for patients, clinicians, and caregivers. Patients often prefer prognostic information in simpler terms like days, weeks, or months [37, 38, 21].
FPN, included for its prior performance evaluation against other measures [25], has lacked independent validation post-publication. Our study confirmed its developmental study findings with a C-index of 0.684 and good calibration. FPN performed comparably to CPS in stratifying patients for 15, 30, and 60-day survival probabilities, although CPS showed slightly better accuracy at 30 and 60 days. However, FPN’s discrimination was lower than PiPS-A or PiPS-B models [21].
PPS, though not designed as a prognostic tool, effectively discriminated survival prospects in a large retrospective study [30]. Lau et al. [30] reported median survivals for PPS levels 10% to 70%, which aligned directionally with our findings, although median survival times differed. Like PPS, CPS also effectively stratified patients into iso-prognostic groups.
PPI, designed to predict 3 and 6-week survival [22], has shown good performance in previous studies [17, 32, 39, 40]. Our study found CPS significantly more accurate than PPI at predicting 3 and 6-week survival (p<0.001), consistent with other comparisons of PPI and CPS [16, 17, 34, 36, 41]. While PPI is designed for 3 and 6-week predictions [34], some studies evaluated its performance at 30, 100, or 90-day survival [16, 17, 36], which is beyond its intended scope.
Our findings suggest caution in adopting prognostic tools over clinical judgment. While none of the tools outperformed CPS, they may still offer valuable clinical practice contributions. Prognostic tools can be more objective, reproducible, and serve as educational aids for less experienced staff or as a second opinion. Clinicians often find prognostication challenging and may avoid specific timeframes, opting for vague estimates. Objective tools can aid in clinical study entry criteria, service case-mix description, and potentially improve communication. Future research should assess the impact of prognostic tools versus CPS on clinical decisions, focusing on ease of use, reliability, and objectivity alongside accuracy.
Acknowledgments
The authors thank the UCL PRIMENT Clinical Trials Unit, Karolina Christodoulides, Jane Harrington, and Florence Todd-Fordham for their contributions. We acknowledge the PiPS2 Investigators and Study Steering Committee members Professor Miriam Johnson, Dr Susan Charman, and Angela McCullagh. Our gratitude extends to all participating patients, carers, clinicians, and collaborators.
Data Availability
Study data will be available in the UCL Research Data Repository (RDR) post-manuscript acceptance.
Funding Statement
This research was funded by the National Institute for Health Research, Health Technology Assessment (HTA) programme (NIHR-HTA 13/20/01). The funders had no role in the study design, data collection, analysis, or manuscript preparation.
References
[References from original article are listed here]
Associated Data
Data Availability Statement
All data files supporting conclusions of this study files will be publically available from the UCL Research Data Repository (RDR) after acceptance of the manuscript.