Depression is a prevalent mental health disorder affecting millions of adults. Early identification and intervention are crucial for effective treatment. This article examines the implementation of VitalSign6, a measurement-based care (MBC) program integrated with a Primary Care Depression Screening Tool, to improve depression screening and treatment in a primary care setting.
The Importance of Depression Screening in Primary Care
The US Preventive Services Task Force recommends screening all adults for depression in primary care settings using evidence-based protocols. Untreated depression leads to significant emotional suffering, reduced productivity, and increased risk of comorbid conditions. Despite these recommendations, a significant number of individuals with depression remain undiagnosed and untreated. The PHQ-2 and PHQ-9 are widely recognized and validated primary care depression screening tools. The PHQ-2, a brief two-question tool, serves as an initial screening step, while the PHQ-9 provides a more comprehensive assessment for individuals who screen positive on the PHQ-2.
Implementing VitalSign6: A Measurement-Based Care Approach
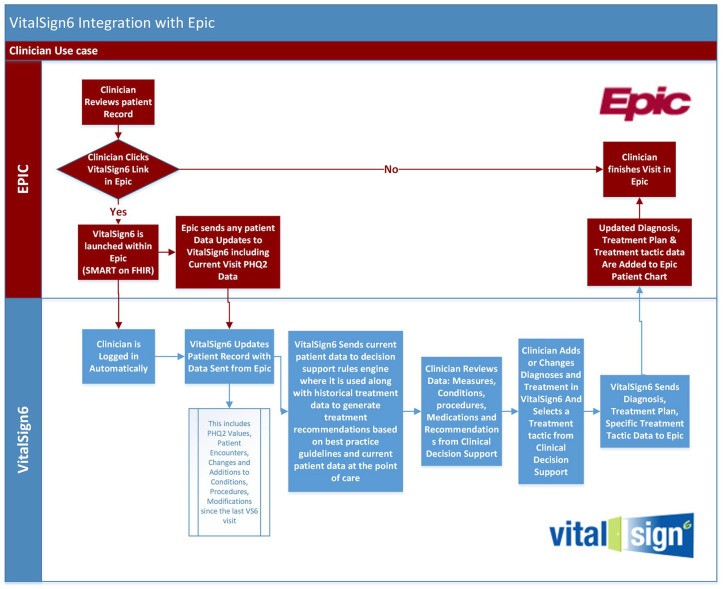
This quality improvement project utilized VitalSign6, an MBC program designed to enhance depression care by incorporating standardized screening tools, treatment protocols, and decision support systems. VitalSign6 integrates with the electronic health record (EHR) system, enabling seamless data transfer and real-time access to patient information. The program was implemented in an academic medical center’s family and community medicine department.
Methodology and Results
A pre-post intervention design was used to evaluate the effectiveness of VitalSign6. Over 95% of the 1200 unique adult patients received the initial PHQ-2 screening. Of those screening positive, a majority completed the PHQ-9. Using this primary care depression screening tool, providers diagnosed and initiated MBC for 236 patients. While follow-up rates were lower than desired, a statistically significant reduction in self-reported depression scores was observed among those who completed follow-up assessments.
Provider and Staff Feedback
Surveys administered to physicians and staff revealed mixed results. While both groups acknowledged the value of the primary care depression screening tool in raising mental health awareness and improving screening rates, concerns were raised about workflow disruptions and technical challenges related to EHR integration. Staff reported increased comfort discussing mental health with patients following training on the MBC program.
Discussion and Conclusion
Integrating a primary care depression screening tool like VitalSign6 with the EHR holds promise for enhancing depression care by facilitating early identification, standardized assessment, and personalized treatment plans. This project demonstrates the potential for MBC programs to improve patient outcomes. However, addressing workflow challenges and optimizing EHR integration are crucial for successful and sustainable implementation. Future research should focus on strategies to improve patient retention in follow-up care and explore the long-term impact of MBC on depression remission rates. This study contributes to the growing body of evidence supporting the effectiveness of VitalSign6 as a valuable tool for managing depression in primary care.