Early integration of palliative care is crucial for patients facing life-limiting illnesses, yet a significant portion of those in need do not receive it. Identifying these patients early in their disease trajectory is paramount to ensuring they receive appropriate care that aligns with their goals and improves their quality of life. However, healthcare systems face considerable challenges in accurately identifying individuals nearing the end of life (EOL) and who would benefit from palliative care services. Clinician prognostication alone has proven to be unreliable, highlighting the need for effective screening tools.
Two primary methods have emerged to aid clinicians in this critical task: the ‘surprise question’ (SQ) and the palliative care screening tool (PCST). The surprise question, a simple yet insightful query – “Would I be surprised if this patient died within the next 6–12 months?” – offers a quick initial assessment without requiring extensive patient data or complex algorithms. While widely used, its accuracy can vary.
The palliative care screening tool (PCST), on the other hand, employs a more structured approach. It gathers patient clinical data, such as functional status and comorbidities, and utilizes a scoring algorithm to estimate survival prognosis. Although both SQ and PCST are valuable tools for identifying patients who may benefit from palliative care, direct comparisons of their effectiveness and the potential benefits of combining them have been limited.
This article delves into the importance of early palliative care identification, explores the utility of palliative care screening tools, and discusses the findings of a study comparing the prognostic accuracy of the surprise question and the palliative care screening tool. Understanding these tools and their applications is essential for healthcare professionals seeking to enhance end-of-life care and ensure timely access to palliative services for patients in need. For those seeking resources and practical tools, a Palliative Care Screening Tool Pdf can be an invaluable asset in implementing these strategies within clinical practice.
Methods and Tools for Palliative Care Screening
The Surprise Question (SQ): A Simple Initial Screen
The surprise question (SQ) serves as a rapid and easily applicable initial screen for identifying patients who may be nearing the end of life. Its simplicity is its strength, requiring minimal time and resources. By prompting healthcare providers to reflect on a patient’s prognosis with the question, “Would I be surprised if this patient died in the next 6–12 months?”, the SQ aims to tap into clinical intuition and identify individuals whose health trajectory suggests a limited prognosis.
While the SQ is valuable as a preliminary step, it is important to acknowledge its limitations. Its accuracy can fluctuate depending on the patient population and the clinician’s experience. It is most effective when used as part of a broader assessment strategy, rather than as a standalone definitive tool.
Palliative Care Screening Tool (PCST): A Data-Driven Approach
The palliative care screening tool (PCST) offers a more systematic and data-driven approach to identifying patients needing palliative care. Unlike the subjective nature of the SQ, the PCST incorporates objective clinical data, including:
- Functional Status: Assessing the patient’s ability to perform daily activities, often using scales like the Eastern Cooperative Oncology Group (ECOG) performance status.
- Comorbidities: Identifying the presence and severity of conditions such as heart failure, chronic obstructive pulmonary disease (COPD), cancer, liver cirrhosis, end-stage renal disease, and dementia.
This data is then processed using a scoring algorithm, often detailed within a palliative care screening tool PDF document, to generate a risk assessment for mortality and palliative care need. The PCST provides a more structured and potentially more objective assessment compared to the SQ.
Combining SQ and PCST for Enhanced Accuracy
Recognizing the strengths and limitations of both the SQ and PCST, research has explored the potential benefits of combining these tools. The hypothesis is that integrating the rapid assessment of the SQ with the data-driven approach of the PCST could lead to improved accuracy in identifying patients needing palliative care.
One study investigated this combined approach, comparing its prognostic accuracy to using either tool in isolation. The findings of this study shed light on the effectiveness of these screening methods and the potential for optimized palliative care identification strategies.
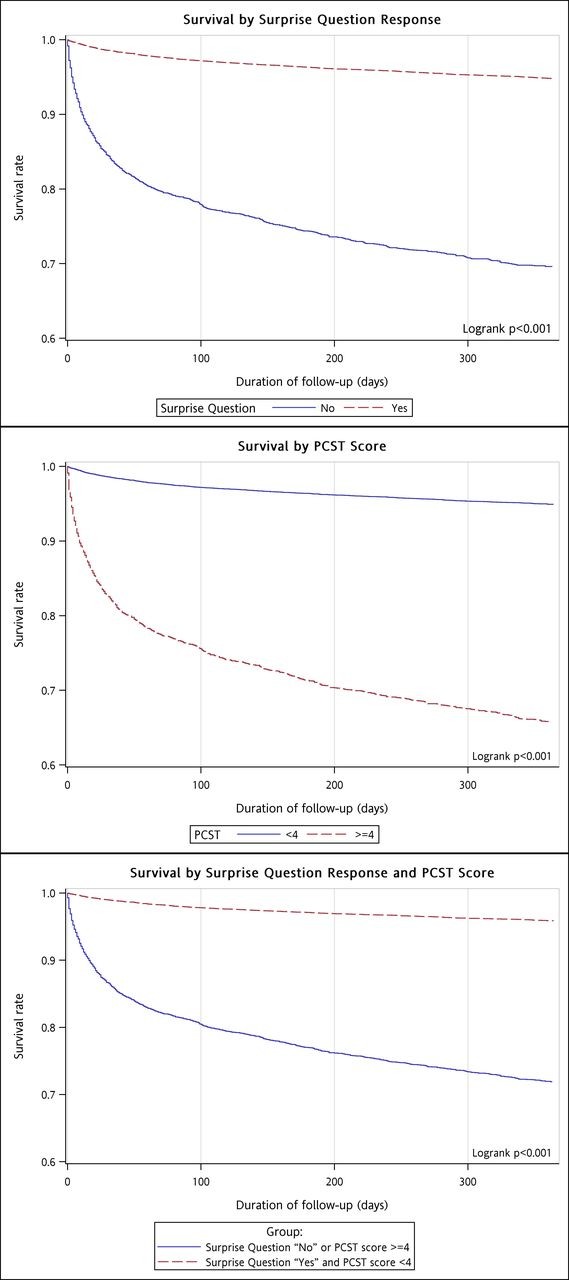 Patients’ survival rate by surprise question response and palliative care screening tool (PCST) scores.
Patients’ survival rate by surprise question response and palliative care screening tool (PCST) scores.
Alt: Kaplan-Meier survival curves illustrating patient survival rates based on surprise question responses and palliative care screening tool (PCST) scores, highlighting differences in survival probabilities across groups.
Study on the Accuracy of SQ and PCST
A cohort study involving 21,109 patients admitted to Taipei City Hospital (TCH) in 2015 was conducted to compare the prognostic accuracy of the surprise question (SQ) and the palliative care screening tool (PCST). This large-scale study aimed to determine the effectiveness of each tool, both individually and in combination, in predicting 12-month mortality.
Study Design and Participants
The study retrospectively analyzed data from patients’ medical records. Patients aged 18 years or older admitted to TCH in 2015 were included, and followed until death or the end of 2016. Nurses at TCH routinely administered both the SQ and PCST to patients upon admission as part of a palliative care program implemented since 2015.
Key Findings
The study yielded significant findings regarding the accuracy of SQ and PCST:
- Individual Accuracy: Both SQ and PCST demonstrated moderate prognostic accuracy, with c-statistics of 0.680 and 0.689, respectively.
- Combined Approach Superiority: The combination of SQ and PCST significantly improved prognostic accuracy, achieving a c-statistic of 0.739. This indicates that utilizing both tools together is more effective than relying on either one alone.
- Sensitivity and Specificity: While both tools showed high specificity (ability to correctly identify patients not at high risk of death), the combined approach significantly increased sensitivity (ability to correctly identify patients at high risk of death) to 59.2%.
- Predictive Values: The negative predictive value (NPV) was high for all approaches, indicating a strong ability to identify patients who were likely to survive. However, the positive predictive value (PPV) was lower, suggesting that while the tools are good at ruling out risk, they are less precise in confirming it.
These results underscore the value of using palliative care screening tools to enhance the identification of patients nearing the end of life. The improved accuracy achieved by combining SQ and PCST suggests a practical and effective strategy for healthcare systems seeking to optimize palliative care delivery.
Implications for Clinical Practice
The findings of this study have important implications for clinical practice and palliative care program implementation. The evidence supporting the combined use of SQ and PCST suggests that healthcare providers should consider integrating both tools into routine patient assessments.
Utilizing a palliative care screening tool PDF that incorporates both the SQ and PCST methodologies can streamline this process. Such a resource can provide:
- Standardized questionnaires: Ensuring consistent application of both screening methods.
- Scoring algorithms: Facilitating accurate risk assessment based on PCST data.
- Guidance for interpretation: Helping clinicians understand the results and make informed decisions about palliative care referrals.
By adopting a systematic screening approach using tools like a palliative care screening tool PDF, healthcare systems can move towards earlier and more accurate identification of patients who would benefit from palliative care, ultimately improving their end-of-life experiences.
Alt: Table summarizing patient characteristics categorized by surprise question response (‘yes’ or ‘no’), detailing demographic data, comorbidities, ECOG performance status, and PCST scores across the groups.
Conclusion: Enhancing Palliative Care with Screening Tools
Early identification of patients in need of palliative care is essential for providing holistic, patient-centered care that addresses their physical, emotional, and spiritual needs. Palliative care screening tools, such as the surprise question (SQ) and the palliative care screening tool (PCST), play a vital role in this process.
This study demonstrates that while both SQ and PCST are valuable individually, their combined use significantly enhances the accuracy of identifying patients nearing the end of life. This improved accuracy translates to a greater opportunity to offer timely palliative care services, aligning care with patient goals and improving the quality of end-of-life care.
For healthcare professionals seeking to implement best practices in palliative care, utilizing a palliative care screening tool PDF that incorporates both SQ and PCST offers a practical and evidence-based approach. By embracing these tools and integrating them into routine clinical workflows, healthcare systems can make significant strides in ensuring that all patients who could benefit from palliative care receive it in a timely and effective manner. Further research should focus on implementation strategies and the long-term impact of using combined screening tools on patient outcomes and healthcare costs.
References
[List of references from the original article, formatted in markdown as links if possible, otherwise as plain text]
[1] Ref 1
[2] Ref 2
[3] Ref 3
[4] Ref 4
[5] Ref 5
[6] Ref 6
[7] Ref 7
[8] Ref 8
[9] Ref 9
[10] Ref 10
[11] Ref 11
[12] Ref 12
[13] Ref 13
[14] Ref 14
[15] Ref 15
[16] Ref 16
[17] Ref 17
[18] Ref 18
[19] Ref 19
[20] Ref 20
[21] Ref 21
[22] Ref 22
[23] Ref 23
[24] Ref 24
[25] Ref 25
[26] Ref 26
[27] Ref 27
[28] Ref 28

