Primary care settings are increasingly becoming the front line of defense in healthcare, offering accessible and continuous medical care to a broad population. Within this vital domain, the integration of comprehensive health services, including routine eye examinations, is gaining significant traction. Eye health is an integral component of overall well-being, and early detection of ocular pathologies can be pivotal in preventing vision loss and managing systemic diseases that manifest in the eyes. For conditions like diabetic retinopathy (DR), a leading cause of blindness, timely screening is not just beneficial but crucial. This article delves into the landscape of Available Eye Exam Tools In Primary Care, examining their role in enhancing patient access to essential vision health services and improving early detection rates for sight-threatening conditions.
The shift towards incorporating eye care within primary care is driven by several compelling factors. Firstly, primary care physicians (PCPs) are often the first point of contact for patients, especially those managing chronic conditions such as diabetes. Integrating eye exams into routine primary care visits can overcome barriers associated with specialist referrals, appointment scheduling, and patient compliance. Secondly, advancements in technology have led to the development of user-friendly and efficient diagnostic tools that can be readily deployed in primary care settings. These tools range from portable retinal cameras to sophisticated telemedicine platforms that facilitate remote expert interpretation. By leveraging these innovations, primary care practices can extend their scope of services and play a more proactive role in preventive eye care.
This exploration will highlight the types of eye exam tools that are currently available and practically applicable in primary care. We will discuss the functionalities, benefits, and considerations for implementing these tools, drawing insights from successful models such as primary care-based teleretina screening programs. The aim is to provide a comprehensive overview for healthcare professionals and decision-makers considering the adoption of eye exam tools in primary care to improve patient outcomes and population health.
Understanding the Need for Eye Exam Tools in Primary Care
The imperative for integrating eye exam tools within primary care stems from the growing burden of eye diseases and the critical role of early detection in preventing vision impairment. Diabetic retinopathy serves as a prime example of a condition where timely screening and intervention can significantly alter the course of the disease. As diabetes prevalence continues to rise globally, so does the number of individuals at risk of developing DR and subsequent vision loss.
Diabetic retinopathy (DR) is a microvascular complication of diabetes that affects the blood vessels in the retina. Over time, chronic hyperglycemia can damage these vessels, leading to a range of retinal abnormalities, from mild non-proliferative DR to severe proliferative DR, which can cause blindness if left untreated. Early stages of DR often have no noticeable symptoms, making routine screening essential for timely diagnosis and treatment. Vision loss from DR is largely preventable with early detection and appropriate management, underscoring the importance of accessible and widespread screening programs.
However, despite the established guidelines recommending annual eye exams for individuals with diabetes, screening rates remain suboptimal in many populations. Several barriers contribute to this gap, including:
- Access to Eye Care Specialists: Traditional DR screening often requires referral to an ophthalmologist or optometrist, which can be challenging due to geographical limitations, long wait times for appointments, and transportation issues, especially for patients in rural or underserved communities.
- Patient Awareness and Compliance: Some patients may not be fully aware of the importance of regular eye exams, particularly if they are asymptomatic. Financial constraints, lack of insurance, and competing healthcare priorities can also deter patients from seeking specialist eye care.
- Healthcare System Silos: Fragmented healthcare systems can hinder effective coordination between primary care and specialist eye care. Referral processes can be cumbersome, and communication of screening results back to PCPs may be inconsistent, leading to missed follow-up and delayed treatment.
Integrating eye exam tools into primary care addresses these barriers by bringing screening directly to the patient within a familiar and accessible setting. By equipping primary care practices with the necessary tools and workflows, we can:
- Improve Screening Rates: Making eye exams a routine part of primary care visits increases the likelihood of screening, particularly for patients who might not otherwise seek specialist care.
- Enhance Early Detection: Earlier detection of DR and other eye conditions allows for timely intervention, which can prevent or slow down disease progression and reduce the risk of vision loss.
- Increase Patient Convenience and Compliance: Offering eye exams within primary care reduces the need for separate appointments, travel, and associated costs, making screening more convenient and patient-friendly.
- Strengthen Primary Care’s Role in Preventive Care: Integrating eye care reinforces the role of primary care as a comprehensive healthcare provider and enhances its capacity to deliver preventive services.
The incorporation of eye exam tools in primary care is not just about increasing screening numbers; it’s about fundamentally shifting towards a more proactive and integrated approach to healthcare delivery. By empowering PCPs with the tools and technologies to conduct basic eye screenings, we can bridge the gap in access to eye care and ensure that more individuals receive the timely attention they need to preserve their vision.
Types of Eye Exam Tools Available for Primary Care
The landscape of available eye exam tools suitable for primary care has evolved significantly, driven by technological advancements that prioritize ease of use, portability, and efficiency. These tools can be broadly categorized into retinal imaging systems, telemedicine platforms, and AI-assisted diagnostic tools, each offering unique capabilities to enhance eye care within primary care settings.
Retinal Imaging Systems
Retinal cameras, also known as fundus cameras, are the cornerstone of eye exam tools in primary care for DR screening and detection of other retinal pathologies. These devices capture digital images of the retina, allowing for detailed examination of the optic nerve, macula, blood vessels, and other retinal structures. Several types of retinal cameras are well-suited for primary care:
-
Non-Mydriatic Fundus Cameras: These cameras can capture retinal images without the need for pupil dilation, making the screening process faster, more comfortable for patients, and easier to implement in a busy primary care setting. Non-mydriatic imaging eliminates the waiting time associated with pupil dilation and avoids potential side effects like blurry vision and light sensitivity.
-
Portable and Handheld Fundus Cameras: Compact and portable retinal cameras are ideal for primary care practices as they require minimal space and can be easily moved between exam rooms or even used in outreach settings. Handheld models offer even greater flexibility and are particularly useful for screening patients with mobility limitations or in community-based programs.
These cameras are designed for ease of use, often featuring automated image capture and user-friendly interfaces that require minimal training for primary care staff. High-quality retinal images captured by these cameras can be stored digitally and transmitted securely for remote interpretation by eye care specialists.
Telemedicine Platforms for Teleretina Programs
Telemedicine platforms are integral to teleretina programs, which leverage technology to facilitate remote DR screening and interpretation. These platforms provide a secure and efficient means to:
-
Transmit Retinal Images: Telemedicine platforms enable the secure transfer of retinal images captured in primary care to a centralized reading center or to remote ophthalmologists/optometrists for interpretation.
-
Manage Workflow and Data: These platforms often include workflow management tools for tracking screenings, managing patient data, and ensuring timely interpretation of images. They can integrate with Electronic Health Records (EHRs) to streamline data entry and retrieval.
-
Facilitate Communication and Reporting: Telemedicine platforms facilitate communication between primary care providers and eye care specialists, allowing for efficient reporting of screening results and recommendations for follow-up care. Automated result notification systems can ensure that PCPs are promptly informed of screening outcomes.
The effectiveness of teleretina programs hinges on the seamless integration of these telemedicine platforms with existing healthcare infrastructure, including EHR and Picture Archiving and Communication Systems (PACS). This integration ensures efficient data flow, reduces manual data entry, and minimizes the burden on healthcare providers.
AI-Assisted Diagnostic Tools
Artificial intelligence (AI) is increasingly being incorporated into eye exam tools, particularly for automated analysis of retinal images for DR detection. AI-powered diagnostic systems offer the potential to:
-
Automate DR Screening: AI algorithms can analyze retinal images and automatically detect signs of DR with high sensitivity and specificity, reducing the need for manual interpretation in many cases.
-
Improve Efficiency and Scalability: Automated AI systems can process a high volume of images rapidly, making them well-suited for large-scale screening programs and areas with limited access to eye care specialists.
-
Provide Point-of-Care Diagnosis: Some AI systems are designed for point-of-care use, providing immediate screening results in primary care settings, enabling faster decision-making and patient management.
While AI in DR screening is still an evolving field, several FDA-approved AI systems are now available, demonstrating the growing maturity and clinical applicability of this technology. These systems can serve as valuable tools to augment human interpretation, particularly in resource-constrained settings or for preliminary screening to triage patients needing further expert evaluation.
Other Potential Eye Exam Tools
Beyond retinal imaging, other eye exam tools can be considered for primary care, depending on the scope of services and specific patient needs. These may include:
- Visual Acuity Charts: Basic visual acuity testing using standardized charts (like Snellen or ETDRS charts) can be easily incorporated into primary care to assess overall vision and identify patients who may require further eye examination.
- Intraocular Pressure (IOP) Measurement Devices: Portable tonometers can be used to measure IOP, a key risk factor for glaucoma. While IOP measurement alone is not sufficient for glaucoma screening, it can be a useful adjunct in identifying individuals who may be at higher risk and warrant referral to an eye specialist.
- Anterior Segment Cameras: While primarily focused on retinal imaging, some fundus cameras can also capture images of the anterior segment of the eye, allowing for basic assessment of conditions like cataracts or corneal abnormalities.
The selection of appropriate eye exam tools for primary care should be guided by the specific goals of the screening program, the resources available, the training capacity of primary care staff, and the need for integration with existing healthcare systems. Often, a combination of tools, such as retinal cameras coupled with telemedicine platforms and potentially AI assistance, offers the most comprehensive and effective approach to enhancing eye care in primary care settings.
Implementing Eye Exam Tools in Primary Care: Lessons from a Teleretina Program
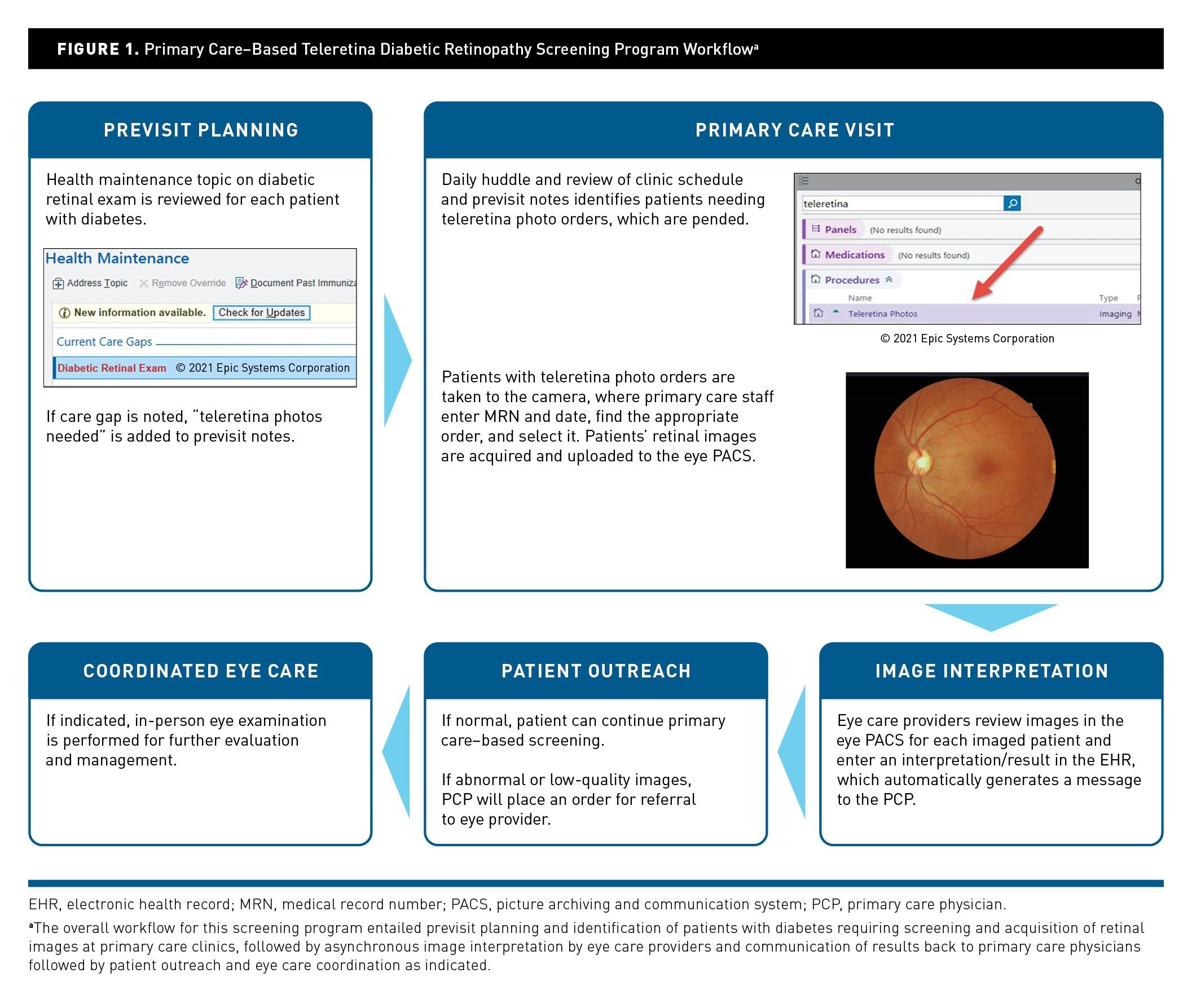
The successful integration of eye exam tools into primary care requires careful planning, workflow design, and attention to health information technology (IT) considerations. The experience of implementing a primary care-based teleretina program at an academic medical center provides valuable insights into the practical aspects of establishing such a program and the role of clinical informatics tools in ensuring its effectiveness.
This program, conducted at the University of California San Diego (UCSD), aimed to improve diabetic retinopathy (DR) screening rates by establishing a teleretina screening workflow within primary care clinics. The key components of the program included:
-
Needs Assessment: A thorough analysis of existing DR screening workflows revealed gaps in in-person eye clinic examinations, highlighting the need for expanding screening to primary care settings. Barriers identified included patient loss to follow-up in scheduling, inappropriate triage at eye clinics, and lack of seamless communication of results back to PCPs.
-
Design Goals for Informatics Tools: Several design goals were established to address the identified gaps and facilitate smooth program implementation:
- Integration with Existing Ophthalmology Viewing Systems: Retinal images acquired in primary care needed to be integrated with the eye clinic’s Picture Archiving and Communication System (PACS) to allow eye care providers to view all images in one place.
- Automated Billing and Charge Capture: To minimize administrative burden, automated billing and charge capture were designed to occur upon image interpretation, with charges automatically distributed between primary care and ophthalmology services.
- Automated Completion of Health Maintenance Topic: To streamline quality metric reporting, the system was designed to automatically complete the EHR’s health maintenance topic on diabetic eye exams upon image interpretation.
- Report for Tracking Screened Patients: A custom report was created to aggregate all teleretina DR screening orders, making it easier for eye care providers to monitor the status of imaging exams and facilitate interpretation completion.
- Macros for Standardizing Imaging Interpretation: Customized image interpretation windows with macros were developed to standardize data entry, facilitate structured reporting, and generate natural language notes easily readable by PCPs.
-
Implementation Processes: Pre-implementation stages involved workflow design, equipment installation, and training for primary care staff on camera use, image acquisition, and the new workflow within PACS and EHR. Testing was performed to ensure successful system integration before go-live. On-site support was provided at go-live, and ongoing stakeholder meetings were conducted to review outcome metrics and address any challenges.
-
Outcomes and Impact: The program screened 316 primary care patients over a 9-month period. A significant proportion (23%) were found to have ocular pathology, including previously undiagnosed DR and other eye conditions. The institutional diabetic eye exam metric improved from 47% to 65% after program implementation, exceeding the predefined goal.
-
Informatics Challenges and Solutions: Despite the program’s success, several informatics challenges emerged post-deployment, requiring iterative solutions:
- Managing Imaging Orders: Uncompleted orders (due to patient decline or staffing constraints) cluttered the screening report. The solution was to instruct primary care staff to cancel uncompleted orders and modify the report to reflect cancellation status.
- Handling Poor-Quality Images: Automated billing and health maintenance completion occurred even for poor-quality images. The solution involved manual removal of charges and narrative text in interpretations for now, with a design modification underway to allow eye care providers to mark orders as “incomplete” for poor-quality images, preventing automated billing and health maintenance completion in such cases.
These experiences underscore the importance of a holistic approach to implementing eye exam tools in primary care, encompassing not only the selection of appropriate technologies but also meticulous workflow design, robust IT infrastructure, comprehensive training, and ongoing monitoring and adaptation. Clinical informatics tools play a crucial role in streamlining workflows, automating administrative tasks, facilitating data management, and ultimately enhancing the efficiency and effectiveness of primary care-based eye screening programs.
Benefits of Using Eye Exam Tools in Primary Care
The integration of eye exam tools into primary care offers a multitude of benefits, extending beyond improved screening rates to encompass enhanced patient access, cost-effectiveness, and better overall diabetes care coordination. These advantages solidify the value proposition of incorporating eye care within the primary care domain.
- Improved Screening Rates and Early Detection: As demonstrated by the UCSD teleretina program and other similar initiatives, deploying eye exam tools in primary care significantly increases DR screening rates. By making screening readily available during routine primary care visits, more patients, especially those who are less likely to seek specialist care, can be screened. This leads to earlier detection of DR and other eye conditions, enabling timely intervention and reducing the risk of vision loss.
- Increased Patient Access and Convenience: Primary care settings are often more geographically accessible and convenient for patients compared to specialist eye clinics. Integrating eye exams into primary care eliminates the need for separate appointments, reduces travel time and costs, and minimizes the burden on patients, particularly those with mobility issues or limited resources. This enhanced accessibility can improve patient compliance with recommended screening guidelines.
- Reduced Healthcare Costs: While the initial investment in eye exam tools and program implementation is necessary, primary care-based screening can be cost-effective in the long run. Early detection and treatment of DR can prevent costly vision loss and associated healthcare expenditures. Telemedicine-based approaches, in particular, can reduce the need for in-person specialist consultations, further contributing to cost savings. Studies have shown the cost-effectiveness of teleretina programs compared to traditional referral-based screening.
- Better Diabetes Care Coordination: For patients with diabetes, integrating DR screening into primary care fosters a more holistic and coordinated approach to diabetes management. PCPs can directly address eye health as part of comprehensive diabetes care, reinforcing the importance of eye exams and facilitating timely referrals to specialists when necessary. Seamless communication between primary care and eye care providers, facilitated by telemedicine platforms and EHR integration, ensures continuity of care and improves patient outcomes.
- Potential for Expanding Screening for Other Eye Conditions: While DR screening is a primary focus, eye exam tools in primary care can also contribute to the detection of other prevalent eye conditions, such as glaucoma, age-related macular degeneration (AMD), and cataracts. Retinal images can be reviewed for signs of these conditions, prompting referrals for further evaluation and management. Expanding the scope of primary care-based eye screening beyond DR can further enhance its public health impact.
The cumulative benefits of using eye exam tools in primary care underscore their potential to transform eye care delivery, making it more accessible, efficient, and patient-centered. By embracing these tools and integrating them effectively into primary care workflows, healthcare systems can make significant strides in preventing vision loss and improving the overall eye health of the population.
Considerations for Choosing and Implementing Eye Exam Tools
Selecting and implementing eye exam tools in primary care is a multifaceted process that requires careful consideration of various factors to ensure successful integration and program sustainability. Key considerations include cost, ease of use and training, system integration, image quality and diagnostic accuracy, and regulatory compliance.
- Cost and Budget: The initial cost of acquiring retinal cameras, telemedicine platforms, and AI-assisted diagnostic systems can be a significant investment for primary care practices or healthcare organizations. It is crucial to conduct a thorough cost-benefit analysis, considering not only the upfront costs but also the potential return on investment in terms of improved screening rates, reduced healthcare costs associated with vision loss, and enhanced revenue through billing for screening services. Exploring funding opportunities, grants, and leasing options can help mitigate the financial burden.
- Ease of Use and Training: Primary care staff may not have specialized training in ophthalmology or retinal imaging. Therefore, it is essential to choose eye exam tools that are user-friendly and require minimal training to operate effectively. Devices with automated image capture, intuitive interfaces, and comprehensive training programs are preferable. Ongoing technical support and refresher training should also be considered to ensure staff competency and address any operational issues.
- System Integration: Seamless integration with existing healthcare systems, particularly EHR and PACS, is critical for efficient workflow and data management. The chosen eye exam tools and telemedicine platforms should be compatible with the practice’s EHR system to facilitate automated data entry, result reporting, and communication. Integration with PACS is important for image storage, retrieval, and remote interpretation by eye care specialists. Interoperability and adherence to healthcare IT standards are key considerations for system integration.
- Image Quality and Diagnostic Accuracy: The quality of retinal images captured by fundus cameras and the diagnostic accuracy of AI-assisted systems directly impact the effectiveness of primary care-based screening. Selecting retinal cameras that produce high-resolution images and AI systems with validated performance metrics is crucial. Regular quality control measures, image quality assessments, and protocols for managing poor-quality images should be implemented to maintain screening accuracy.
- Regulatory Compliance and Data Security: Implementing eye exam tools and telemedicine platforms must comply with relevant healthcare regulations, including HIPAA in the United States, and data privacy laws. Ensuring secure data transmission, storage, and access is paramount to protect patient privacy and confidentiality. Choosing vendors that are HIPAA compliant and implement robust security measures is essential. Additionally, compliance with billing and coding regulations for telehealth and DR screening services should be ensured.
Beyond these technical and operational considerations, successful implementation also requires stakeholder engagement, workflow optimization, and ongoing monitoring and evaluation. Engaging primary care providers, staff, eye care specialists, and IT personnel in the planning and implementation process is crucial to ensure buy-in and address any concerns. Optimizing workflows to integrate eye exams seamlessly into routine primary care visits and establishing clear protocols for image acquisition, interpretation, and follow-up are essential for program efficiency. Regular monitoring of screening rates, image quality, diagnostic accuracy, and patient outcomes, along with ongoing program evaluation and adaptation, are necessary for continuous improvement and long-term sustainability.
Conclusion
The integration of available eye exam tools in primary care represents a significant advancement in healthcare delivery, offering a practical and effective approach to enhance patient access to vital eye care services. By leveraging user-friendly retinal imaging systems, telemedicine platforms, and emerging AI-assisted diagnostic tools, primary care practices can play a more proactive role in preventive eye care, particularly for conditions like diabetic retinopathy.
The benefits of this integration are manifold, encompassing improved screening rates, earlier disease detection, increased patient convenience, reduced healthcare costs, and better coordination of care, especially for individuals with diabetes. Experiences from successful teleretina programs highlight the importance of careful planning, robust IT infrastructure, comprehensive training, and ongoing program management in realizing these benefits.
As technology continues to evolve and healthcare delivery models adapt to meet the changing needs of populations, the role of primary care in providing expanded services, including eye care, will only become more critical. Embracing available eye exam tools and integrating them thoughtfully into primary care settings is not just a technological upgrade; it is a strategic step towards a more accessible, equitable, and effective healthcare system that prioritizes preventive care and patient well-being. By empowering primary care providers with the right tools and support, we can collectively work towards a future where vision loss from preventable eye diseases is significantly reduced, and everyone has the opportunity to maintain healthy vision throughout their lives.