Clinical audits are crucial for evaluating and enhancing the quality of care in healthcare settings. This process involves comparing current practices against established standards to identify areas needing improvement. This guide explores the principles of clinical audits, focusing on their application in nephrology and highlighting their broader potential in improving care services.
Defining Clinical Audits and Their Purpose
A clinical audit is a systematic process that measures clinical outcomes and processes against pre-defined, evidence-based standards. This comparison helps pinpoint discrepancies and informs strategies for enhancing care quality. Unlike research, which explores unknown territories, audits assess current practices against known benchmarks. The ultimate goal is to elevate patient care through improved clinician knowledge, problem-solving, standardized practices, and bridging the gap between theory and real-world application.
Key Steps in Conducting a Clinical Audit
A successful clinical audit involves a cyclical process with five key steps:
1. Preparation: Laying the Groundwork
Thorough preparation is paramount. This includes:
- Topic Selection: Choosing a clinically significant, measurable, and impactful issue. High-volume, high-cost, high-risk, highly variable, complex, or innovative areas are ideal candidates.
- Defining Objectives: Clearly stating the audit’s goals, such as implementing new protocols or refining existing ones.
- Resource Allocation: Securing necessary resources, including personnel, data collection tools, and training. A multidisciplinary team tailored to the audit topic is crucial.
2. Establishing Standards and Intervention Strategies
This step involves:
- Defining Indicators, Criteria, and Standards:
- Indicator: A measurable variable reflecting changes related to defined criteria.
- Criterion: A definable and measurable aspect of healthcare quality, outlining expected outcomes based on good practice.
- Standard: The desired level of care for each criterion, often expressed as a percentage representing the acceptable threshold.
- Choosing Reliable Sources: Basing standards on international guidelines, scientific literature, expert consensus, and data from comparable facilities ensures credibility.
- Developing Intervention Strategies: Pre-defining clear, actionable steps to address discrepancies identified during the audit.
3. Data Collection: Gathering Evidence
Data can be collected prospectively or retrospectively:
- Prospective Audits: More time-consuming but offer greater accuracy and a realistic depiction of current practices.
- Retrospective Audits: Faster but potentially reliant on less comprehensive historical data.
Regardless of the method, meticulous planning of variables, analysis methods, and data collection tools (e.g., specifically designed forms or databases) is essential. Sampling techniques may be necessary for large patient populations. Patient privacy must be prioritized throughout this process.
4. Data Analysis and Corrective Actions
This crucial phase involves comparing collected data with established standards. Open communication and a non-judgmental approach are key to objective analysis. Outcomes can lead to:
- Standard Met: Implementation of monitoring strategies to maintain achieved levels.
- Standard Not Met: Determining feasibility of improvement. If achievable, identifying barriers and developing corrective actions based on pre-defined strategies. Dissemination of educational materials alone is often insufficient; implementation methods like training and peer discussions are crucial.
5. Verification and Maintenance: Ensuring Long-Term Improvement
This final step involves:
- Regular Monitoring: Periodically assessing the impact of implemented changes using methods comparable to the initial data collection.
- Adapting Strategies: Modifying interventions if objectives are not met.
- Sustaining Improvements: Continuous monitoring even after success to ensure long-term maintenance of improved practices.
Clinical Audits in Nephrology: Practical Applications
Clinical audits have been widely applied in nephrology, particularly in hemodialysis settings. Areas of focus include:
- Vascular Access Management: Optimizing access choices to reduce central venous catheter use.
- Hypertension Management: Investigating factors influencing blood pressure control, such as dialysate sodium concentration and temperature.
- Mineral Metabolism Disorders: Identifying barriers to achieving therapeutic targets and developing strategies to improve management.
These audits demonstrate the potential of this methodology in identifying and addressing critical issues in nephrology, leading to significant improvements in patient care. One study showed that the mere announcement of an audit on hypertension management led to a decrease in prevalence, highlighting the inherent motivational aspect of this process.
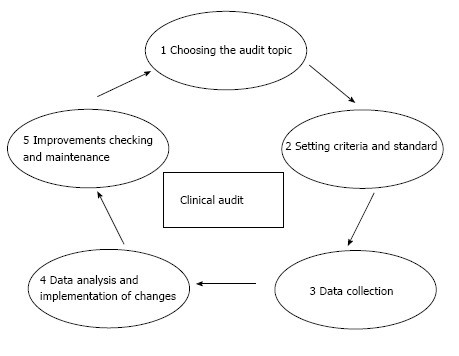 Figure 1
Figure 1
Expanding the Scope: Future Applications of Auditing Tools
The principles of clinical audits can be applied to various areas within nephrology and beyond:
- Peritoneal Dialysis: Addressing treatment failure and reducing infection rates.
- Kidney Transplantation: Streamlining waiting list processes.
- General Patient Care: Managing dyslipidemia, promoting lifestyle changes, and optimizing medication prescription.
Conclusion: Auditing Tools – Essential for Quality Care
Clinical audits are invaluable tools for continuous quality improvement in care services. Their systematic approach allows for objective assessment, identification of areas for improvement, and implementation of targeted interventions. While evidence supports their efficacy, further research can solidify their role in various healthcare settings. Wider adoption and integration of clinical audit methodologies, supported by clear guidelines and training, are crucial to maximizing their potential in enhancing patient care across diverse medical disciplines. The checklist presented in the original article provides a practical framework for planning and implementing effective clinical audits.
